PET/CT imaging with a new radiotracer (F-18 PSMA-1007) is superior to MRI prior to surgery in men with intermediate-risk and high-risk prostate cancer, according to a study published on July 1 in JAMA Oncology.
In 134 participants in a phase II trial, F-18 PSMA-1007 PET/CT was more accurate in identifying final tumor stages before patients underwent radical prostatectomies, noted lead author Nikhile Mookerji, MD, of the University of Alberta in Edmonton, Alberta, Canada, and colleagues.
"F-18 PSMA-1007 PET/CT provided improved accuracy compared with multiparametric MRI for prostate cancer tumor staging before radical treatment," the group wrote.
The diagnosis and management of intermediate-risk and high-risk prostate cancer are increasingly informed by advances in diagnostic imaging, the authors noted. Current guidelines recommend the use of multiparametric MRI to assist with diagnosis and locoregional staging of prostate cancer before radical prostatectomy.
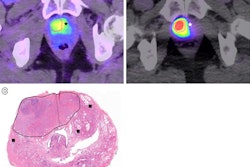
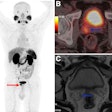
In small studies, F-18 PSMA-1007 PET/CT has shown promise as a more accurate approach based on its ability to reveal prostate-specific membrane antigen (PSMA) on the surface of cancer cells. In this phase II clinical trial, the researchers sought to evaluate the approach further.
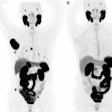
Participants underwent both F-18 PSMA-1007 PET/CT and multiparametric MRI within 14 days of one another and at least five days before surgery at two hospitals in Alberta, Canada. The primary outcome was the correct identification of the prostate cancer tumor stage, which is crucial for surgeons to determine the extent of the disease -- whether it has spread beyond the prostate gland, for instance.
Out of 150 men who participated, 134 ultimately underwent radical prostatectomies (the mean age was 62 years old). Radiologists and nuclear medicine physicians analyzed the images, with their reads ultimately compared to laboratory results from biopsies.
According to the analysis, F-18 PSMA-1007 PET/CT scans alone enabled the identification of the final pathological tumor stage in 61 men (45%) compared to 38 men (28%) with multiparametric MRI, a statistically significant difference, the authors wrote.
While accurate tumor staging was seen in only approximately half of the PSMA-PET scans and one-quarter of MRI scans, the authors attributed this result to the study readers being blinded to the biopsy results, which they noted would be available to physicians planning surgeries in standard clinical settings.
Ultimately, based on the findings, as well as those from previous studies, adopting a single preoperative PSMA-PET scan could potentially replace the trio of conventional imaging tests currently ordered for these patients (MRI, CT abdomen and pelvis, and bone scan), the authors suggested. Moreover, none of the 150 men who underwent both imaging tests experienced an adverse event, which is important if PSMA-PET is to be expanded to patients at earlier stages of the disease, they added.
"Future research should address the accuracy of combining PET/CT and MRI as well as cost-effectiveness of PET/CT for the primary staging of men with prostate cancer," the group concluded.
The full study is available here.