A new delivery route for theranostic agents via arteries rather than intravenous injections could dramatically increase their effect on tumors in patients with prostate cancer, suggests research published August 13 in Radiology.
In a proof-of-concept study, a group at the University of California San Francisco (UCSF) found that uptake by tumors was dramatically higher when gallium-68 (Ga-68) prostate-specific membrane antigen (PSMA)-11 was delivered to patients via prostate arteries versus intravenously.
“Using dynamic PET/CT, selective prostatic arterial infusion of [Ga-68 PSMA-11] resulted in greater tumor standardized uptake values than intravenous infusion in study participants with high-risk prostate cancer,” wrote lead author Ryan Kohlbrenner, MD, and colleagues.
Theranostic pairs are comprised of a common ligand that binds to receptors on cancer cells. The ligands can carry both an imaging agent for first visualizing tumors and then a therapeutic radiopharmaceutical that kills the cells. In the case of Pluvicto, for instance, the common ligand is PSMA, with Ga-68 PSMA-11 being the imaging agent and lutetium-177 PSMA-617 the therapeutic agent, the authors explained.
Conceptually, the group proposed the idea that enhancing tumor uptake of Ga-68 PSMA-11 could serve as a simulation for enhancing therapy with lutetium-177 PSMA-617. In this study, they took the first step and tested a new approach for delivering Ga-68 PSMA-11.
The researchers enrolled five men ages 58, 61, 64, 66, and 68 with untreated, localized prostate cancer (vs. metastatic) between January 2022 and February 2023. Participants underwent two dynamic Ga-68 PSMA-11 PET/CT scans one week apart. During the first scan, the radiotracer was administered intravenously and during the second, the radiotracer was delivered into either the right or left prostatic artery through an angiographically placed microcatheter.
For outcomes, the researchers primarily assessed the maximum standardized uptake value (SUVmax) and mean SUV (SUVmean) of Ga-68 PSMA-11 in prostate tumor volumes of interest (VOIs).
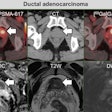
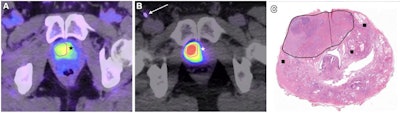 Dynamic PET/CT and pathologic images for a 66-year-old male participant. (A) Axial dynamic PET/CT image acquired during intravenous administration of Ga-68 PSMA-11 demonstrates the hypermetabolic primary prostatic tumor. The right-sided portion of the lesion used for volume of interest (VOI) analysis is outlined in pink, reflecting the margins seen on a prior T2-weighted MRI scan. Tumor radiotracer uptake extends across midline into the left anterior apex (*). (B) Axial dynamic PET/CT image acquired during selective right prostatic arterial administration of Ga-68 PSMA-11 demonstrates intense radiotracer uptake in the VOI outlined in pink. There is comparatively minimal uptake in the unperfused left-sided portion of the tumor (*). The arterial sheath and catheters in the right groin are partially visualized (arrow). (C) Photomicrograph (hematoxylin-eosin stain; unmagnified) of the prostatic apex after radical prostatectomy. The midline (dotted line) and dominant tumor margins (solid line) are shown. Small additional areas of carcinoma (■) without T2-weighted MRI correlates were also identified at pathologic examination. Image and caption courtesy of the RSNA.
Dynamic PET/CT and pathologic images for a 66-year-old male participant. (A) Axial dynamic PET/CT image acquired during intravenous administration of Ga-68 PSMA-11 demonstrates the hypermetabolic primary prostatic tumor. The right-sided portion of the lesion used for volume of interest (VOI) analysis is outlined in pink, reflecting the margins seen on a prior T2-weighted MRI scan. Tumor radiotracer uptake extends across midline into the left anterior apex (*). (B) Axial dynamic PET/CT image acquired during selective right prostatic arterial administration of Ga-68 PSMA-11 demonstrates intense radiotracer uptake in the VOI outlined in pink. There is comparatively minimal uptake in the unperfused left-sided portion of the tumor (*). The arterial sheath and catheters in the right groin are partially visualized (arrow). (C) Photomicrograph (hematoxylin-eosin stain; unmagnified) of the prostatic apex after radical prostatectomy. The midline (dotted line) and dominant tumor margins (solid line) are shown. Small additional areas of carcinoma (■) without T2-weighted MRI correlates were also identified at pathologic examination. Image and caption courtesy of the RSNA.
According to the findings, the mean SUVmax within tumor VOIs was 14 (range, 3 to 43) for venous sessions and 938 (range, 460 to 1436) for arterial sessions (p = 0.008). The SUVmean within VOIs was greater during arterial sessions (p < 0.001) overall and 46-fold and 19-fold greater at peak uptake and final time points, the group reported.
“We demonstrated that the mean maximum standardized uptake value (SUV) was nearly 66-fold higher with selective prostatic intra-arterial administration than intravenous infusions (938 vs. 14) when using [Ga-68 PSMA-11],” the researchers wrote.
Ultimately, this was a proof-of-concept study and the first time selective arterial radioligand infusion for localized prostate cancer has been evaluated, the researchers wrote. Special considerations regarding dosimetry will be required, for instance, as administering PSMA-617 amounts that exceed the target tissue binding capacity will result in systemic circulation of the radioligand, they noted.
“Further study of local-regional, intra-arterial delivery of a PSMA-targeted theranostic agent is warranted in high-risk prostate cancer,” the group concluded.
The full study can be accessed here.