A new PET radiotracer could offer a viable strategy for detecting primary tumors, involved lymph nodes, and distant metastases in patients with clear cell renal cell carcinoma (ccRCC), according to a study published November 14 in the Journal of Nuclear Medicine.
In a so-called “translational” study, a group in China first synthesized the compound (named NYM046) and labeled it with gallium-68 (Ga-68). Next, they verified that it targets ccRRC in mice and then tested it in humans, with promising results.
“Ga-68 NYM046 provides a promising method for diagnosing and monitoring treatment efficacy in patients with ccRCC,” noted lead author Kequan Lou, MD, of the Affiliated Hospital of Jiangnan University in Wuxi, and colleagues.
F-18 FDG is the most commonly used radiotracer for diagnosing tumors in nuclear medicine, yet its performance in diagnosing primary ccRCC tumors has been “disappointing,” the authors explained, as studies suggest its sensitivity is only 62%. Thus, researchers are seeking to develop more effective radiotracers.
The NYM046 molecule the group developed in this study binds to a cell-surface enzyme highly expressed on ccRCC cancer cells called carbonic anhydrase IX (CAIX). Labeling the molecule with the radioisotope Ga-68 forms the radiotracer, which is then detected by PET scanners at the site of tumors when the agent is injected into subjects.
Using a small-animal PET/CT scanner, the researchers first analyzed the biodistribution of Ga-68 NYM046 in mice with xenograft ccRCC tumors and observed high uptake of the tracer by the tumors. They also compared the results to mice imaged with F-18 FDG and noted significantly higher uptake for Ga-NYM046.
The study in humans included 12 participants with confirmed primary or metastatic ccRCC (median age, 59 years old; 9 men and 3 women). Each patient underwent both Ga-68 NYM046 and F-18 FDG PET/CT imaging within three days. Two nuclear medicine experts evaluated the sets of images.
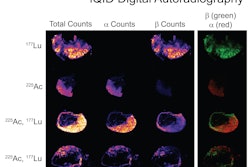
 Representative maximum-intensity projections of five patients (patients 3, 5, 7, 10, and 11) comparing Ga-68 NYM046 and F-18 FDG. Both tracers showed specific retention in bone and lymph node metastases (patients 10 and 11). Ga-68 NYM046 PET/CT outperformed F-18 FDG PET/CT in detecting primary tumors, lung metastases, and pleural metastases (patients 3, 5, 7, and 11). Image available for republishing under Creative Commons license (CC BY 4.0 DEED, Attribution 4.0 International) and courtesy of the Journal of Nuclear Medicine.
Representative maximum-intensity projections of five patients (patients 3, 5, 7, 10, and 11) comparing Ga-68 NYM046 and F-18 FDG. Both tracers showed specific retention in bone and lymph node metastases (patients 10 and 11). Ga-68 NYM046 PET/CT outperformed F-18 FDG PET/CT in detecting primary tumors, lung metastases, and pleural metastases (patients 3, 5, 7, and 11). Image available for republishing under Creative Commons license (CC BY 4.0 DEED, Attribution 4.0 International) and courtesy of the Journal of Nuclear Medicine.
The imaging revealed nine primary tumors, 96 involved lymph nodes, and 147 distant metastases in total. Compared with F-18 FDG PET/CT, Ga-68 NYM046 PET/CT detected more primary tumors (nine versus one), involved lymph nodes (95 vs. 92), and distant metastases (137 vs. 127).
In addition, in a quantitative analysis, the researchers found that maximum standard uptake (SUVmax) values were significantly higher for Ga-68 NYM046 in primary tumors (median, 13.5 vs. 2.4), yet lower in the involved lymph nodes (median, 5.9 vs. 7.6). No significant differences were found for distant metastases among the tracers.
“In a prospective study of 12 patients with ccRCC, Ga-68 NYM046 PET/CT was superior to F-18 FDG PET/CT in the diagnosis of primary tumors and comparable in the detection of metastatic lesions,” the group wrote.
Importantly, no adverse reactions were observed in the patients over a two-week follow-up period, the authors noted.
Ultimately, this is early research, and the study’s small sample of patients may have introduced statistical bias, the researchers wrote. Also, because of the potential side effects of invasive biopsies, the metastatic lesions in the patients were not pathologically confirmed, they added.
“We anticipate addressing these issues in future research,” the group concluded.
The full study is available here.