An FDG-PET scan can separate patients with Alzheimer’s disease from those who have dementia brought on by other illnesses, according to a study in the Journal of Nuclear Medicine. A multi-institutional team used FDG-PET to track bilateral temporo-parietal hypometabolism in patients with hard-to-characterize memory loss, and found that the technique significantly enhanced clinical exams.
The group, led by Dr. John Hoffman from the National Cancer Institute in Bethesda, MD, also went a step farther than previous functional imaging studies by confirming the results with pathology.
In the study sample, 22 patients from the Memory Disorder Clinic at Duke University in Durham, NC, underwent standard FDG-PET brain scans with either the ECAT III from CTI, Knoxville, TN, or the 4096 Plus by GE Medical Systems of Waukesha, WI.
"We administered 370 MBq (10 mCi) FDG followed by a 40-minute uptake period during which the patient remained quiet in a dimly lit room," they wrote. "Transaxial imaging of the entire intracranial contents was obtained. Resting-state FDG-PET scans were obtained and were visually graded by an experienced nuclear medicine physician for the presence of classic bilateral temporo-parietal hypometabolism seen in Alzheimer’s type dementia," (Journal of Nuclear Medicine, November 2000, Vol. 41:11, pp.1920-1928).
The images were then graded on a five-point scale, with zero indicating a normal metabolic pattern, three representing classic bilateral temporo-parietal hypometabolism, and four indicating an abnormal pattern not resulting from Alzheimer’s disease (AD).
Based on the PET data, possible or probable AD was determined as the primary cause of dementia in 12 out of 22 patients. The sensitivity of FDG-PET for tracking hypometabolism was 93%, the specificity was 63%, and the accuracy was 82% in patients with a single pathology, the group reported. In patients with two pathologic diagnoses present, the sensitivity of the scan was 87%, the specificity was 62%, and the accuracy was 81%.
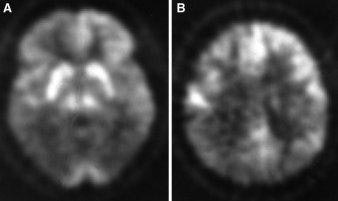
FDG-PET scans of 60-year-old man with a Creutzfeldt-Jakob disease. Note marked reduction in FDG uptake in temporo-parietal image at left, and parietal region, right (JNM, November 2000, Vol.41:11, p.1924).
In two cases, the pathologic diagnosis included AD and another pathologic diagnosis, the authors wrote. In one patient, the clinical diagnosis was probable Alzheimer’s disease and the pathologic diagnosis was AD with Lewy bodies. However, the PET score was consistent with classic AD. In the second case, the clinical diagnosis was progressive supranuclear palsy (PSP) and the pathologic diagnosis was PSP and AD, but the PET scan was rated as a four.
In two other patients, the PET scan was labeled as AD although the pathologic diagnosis did not correspond. In one case, the patient had Creutzfeldt-Jakob disease, which can mimic the metabolic pattern in Alzheimer's disease. The second patient was diagnosed with Lewy bodies.
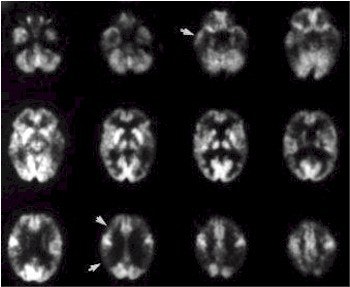
FDG-PET scan of woman, 54, with progressive dementing illness. Note significant reduction in FDG in parietal, temporal, and frontal cortices indicated by arrows. The metabolic pattern of this patient would be considered classic for AD (JNM, November 2000, Vol.41:11, p.1923).
"This study was not specifically designed to show the superiority of FDG-PET metabolic imaging versus careful clinical evaluation in diagnosing AD," the investigators wrote. However, "our results in this group of patients who were difficult to diagnose clinically are certainly encouraging because the FDG-PET diagnostic accuracy noted was better than the clinical result, and, in many instances, the FDG-PET findings were correct and would have provided valuable diagnostic information."
In an accompanying editorial, Dr. Daniel Silverman and Dr. Michael Phelps from the University of California, Los Angeles praised the study for addressing "an issue of pressing clinical relevance: the establishment of reliable estimates of diagnostic accuracy of FDG-PET…."
"If PET [scans] had been interpreted in light of the available clinical information (as would likely occur in its routine clinical application), rather than blindly (as done here to address a specific research question), a diagnostic specificity of 100% would pertain," the editorialists wrote.
The study could advance the development of universally accepted criteria for clinical, radiologic, and pathologic correlation of AD, the authors concluded.
By Shalmali PalAuntMinnie.com staff writer
November 7, 2000
Related Reading
Adding SPECT, MRI to Alzheimer's work-up costs more than it's worth, analysts say,October 11, 2000
Let AuntMinnie.com know what you think about this story.
Copyright © 2000 AuntMinnie.com




















