SAN FRANCISCO - Accurate presurgical staging is crucial for patients with locally invasive bladder cancer, whose long-term survival may also be enhanced with adjuvant chemotherapy after radical cystectomy. Still, the positive nodes must be found before they can be treated, and in this pursuit, a new SPECT/CT imaging method offers hope of improving the odds.
In a poster presentation at this week’s American Urological Association meeting, Dr. Amir Sherif from Uppsala University in Sweden talked with AuntMinnie.com about a new fusion technique that more than doubled the sensitivity of planar lymphoscintigraphy alone. The group's study sought to combine CT imaging with planar lymphoscintigraphy for presurgical planning in patients scheduled for radical cystectomy.
Imaging accuracy key to planning, staging, management
The prognosis for bladder cancer patients, who typically present with painless hematuria, is highly dependent on the type of cancer and disease stage at diagnosis. The most common type, transitional cell carcinoma (TCC), accounts for about 90% of all cases. Squamous cell carcinomas (about 8%) are more invasive, tending to spread deeper into the bladder muscles and beyond. Adenocarcinomas, accounting for 1%-2% of cases, are also more invasive than TCCs.
Overall, 94% of patients with superficial disease can be expected to live five years or more, according to American Cancer Society statistics, though recurrence is common. Five-year survival drops to 49% for those with invasive local disease, and as low as 6% in cases where the cancer has spread to other organs. Some 15,600 new cases are expected to be diagnosed in the U.S. in 2004, and an estimated 8,780 patients will die from the disease.
"In order to reduce the mortality we try to give (patients) adjuvant chemotherapy postoperatively if they have positive nodes," Sherif told AuntMinnie.com. "But if you have a defective method to find the nodes, and you don’t find the nodes during surgery, you will misstage them as n=0. But if you have a method which detects the positive nodes in unexpected areas, then you will have a much more enhanced N staging, and you can really pinpoint those patients (who will benefit from) chemotherapy. In the long run, once you have very effective adjuvant chemotherapy you will probably have better survival."
In the study, six consecutive patients (four men and two women, ages 59-75) with locally invasive bladder cancer underwent SPECT/CT fusion imaging on a Millennium VG5/Hawkeye imaging system (GE Healthcare, Waukesha, WI). Eight additional patients have been included since the study poster was prepared.
SPECT imaging immediately followed by CT was performed five hours after transurethral injection of Albures technetium-99m (60 MBq, divided into four parts) in the detrusor muscle near the tumor site. Optimal waiting times are shorter with Nanocol, another technetium carrier, Sherif said.
The lymphoscintigraphy and CT images were fused using a GE Entegra workstation, and the images compared to each other. Fusing the images with the experimental protocol took the radiologist about two hours per patient, Sherif said.
Sherif, a surgeon, performed the radical cystectomies with extended lymphadenectomy, using peroperative detection of lymph nodes with the gamma probe, as well as visual detection of a dye marker to find the positive nodes.
The fusion process, while time-consuming, enabled detailed preoperative evaluation, Sherif said. According to the results, 20 sentinel nodes were detected in 5/6 patients, compared to two sentinel nodes in six patients visualized using planar lymphoscintigraphy alone. Five of six metastatic sentinel nodes in invasive bladder cancer were seen using the fusion protocol, while lymphoscintigraphy detected only 1/6 nodes containing metastases.
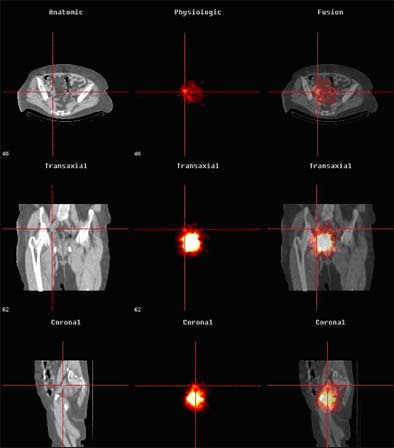 |
| Above, anatomic (CT, left), physiologic (SPECT, middle) and fused images (right) are seen in a bladder cancer patient with sentinel lymph nodes. Images courtesy of Dr. Amir Sherif. |
Overall, planar lymphoscintigraphy alone versus CT-enhanced lymphoscintigraphy detected two and 21 positive nodes, respectively, including 1/2 in patient 1, 0/6 in patient 2, 0/6 in patient 3, 0/4 in patient 4, 1/3 in patient 5, and 0/0 in patient 6, according to the results. Of these, only two positive nodes were detected by the blue dye marker, while the gamma probe detected 10 positive nodes peroperatively. Harvested nodes per patient ranged from six to 24, the total number of detected sentinel nodes per patient ranged from zero to six. All six patients were staged T2.
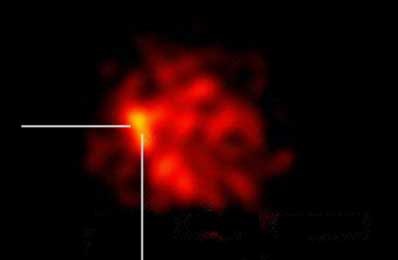 |
| Above, two sentinel lymph nodes are detected over the common iliac artery, right side. Histopathology showed that one contained micrometastatic deposits of urothelial bladder carcinoma. |
"The (combined) system is very accurate for localizing the nodes," Sherif said. "Previously we used only planar lymphoscintigraphy with a gamma camera preoperatively, and we had a much lower yield of detected nodes. By using the fused picture with CT/SPECT, we get a much higher yield, first a higher yield of lymph nodes which are considered to be sentinel nodes, and secondly we find anatomical localization (to be) very accurate."
The results are very similar in the eight patients imaged since the poster was prepared, he said. "A lot of nodes were found in very aberrant localizations, with metastatic deposits where we didn’t expect to find them. And we find them exactly where the radiologist tells us they are."
Sherif hasn’t performed MR lymphography with the new blood-pool contrast agents yet, but said that SPECT/CT confers a major advantage over MRI: While MRI images can be used as guidance during surgery, the SPECT half of the fusion method can be taken right into the OR.
"With this system you do a preoperative picture, and peroperatively you are looking with a gamma detector in the actual operating theater during surgery," he said. "It’s a logical continuation of the preoperative procedure because you’re looking for the same nodes."
By Eric BarnesAuntMinnie.com staff writer
May 12, 2004
Related Reading
Ultrasound aces search for ureteral stones, March 7, 2004
Fluorescence cystoscopy improves detection of early bladder cancer, February 7, 2004
US calculates splenic volume within ten minutes, January 19, 2004
US combo boosts detection, characterization of perianal inflammation, January 15, 2004
Copyright © 2004 AuntMinnie.com




















