
The routine breast imaging workup at two institutions in Belgium involves palpation, mammography, ultrasound, and fine-needle aspirations (FNA) if an abnormality is found. But what do the clinicians do when this chain of tests still yields inconclusive or contradictory results?
"This population represents a daily challenge for the breast imaging community," said Dr. Isabelle Mathieu and colleagues. "In our institutions ... additional methods such as scintimammography or MRI are ordered ... as a second-line imaging technique" (Journal of Nuclear Medicine, October 2005, Vol. 46:10, pp. 1574-1581).
Thus far, scintimammography's value has been proved in women with dense breasts or those who have breast cancer recurrence. Mathieu's group, from Clinique Sainte-Elisabeth in Namur and Cliniques Universitaires Saint-Luc in Brussels, decided to consider the impact of scintimammography in a routine clinical setting, as well as its effect on clinical management. The inclusion criteria for this retrospective study were the complexities of each case rather than a single clinical question as in previous research, the group explained.
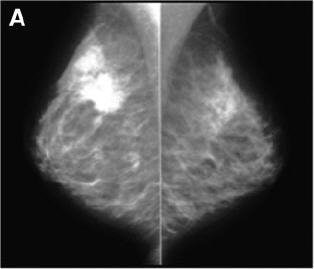 |
| Above, x-ray mammogram, profile views. Polycystic dysplasia of both breasts. On left, suspicious lesion in supra-areolar region of right breast, corresponding to ductal carcinoma on FNA. On right, left breast is dense, especially in superoexternal part of gland. Multiple cysts are seen with ultrasound but no suggestive lesion was evident. |
The team reviewed the files of 104 women (mean age 57 years) who underwent 118 scintimammography procedures in addition to SPECT, planar imaging, and, of course, the traditional workup. If a patient had undergone large-core biopsy, scintimammography was performed at least two weeks later to avoid false-positive results from inflammation.
The cases were organized into four groups:
- Group 1: initial diagnosis of malignancy
- Group 2: suspicion of tumor recurrence
- Group 3: assessment of multicentricity
- Group 4: search for primary tumor in patients with axillary lymph nodes
For scintimammography, SPECT, and planar imaging, 740 MBq of Tc-99m MIBI was administered. An increase in radiotracer uptake or a hot spot in the axillar region was considered positive for tumor.
According to the results, the sensitivity of scintimammography with SPECT (SM-SPECT) was 89% and patient management was altered in 49% of the cases. SM-SPECT was particularly good for diagnosing lobular carcinoma with a sensitivity of 86%.
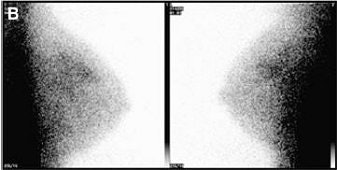 |
| Above, scintimammography (planar lateral views) shows bilateral uptake (left, right breast; right, left breast). Below, axial SPECT views show bilateral lesions (arrows). SPECT allowed precise localization of tumors and oriented large-core biopsy of left breast lesion (open arrow, invasive ductal carcinoma). |
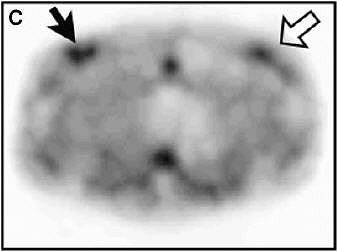 |
| Isabelle Mathieu, Stéphane Mazy, Bernard Willemart, Michel Destine, Gilbert Mazy, and Max Lonneux. "Inconclusive Triple Diagnosis in Breast Cancer Imaging: Is There a Place for Scintimammography?" J Nucl Med 2005; 46;1574-1581, Figure 1. |
The sensitivity for scintimammography alone was 88.4% and the specificity was 67%. SPECT alone found 11 cancers and was significantly more sensitive than planar imaging, although the latter was more specific, the authors stated.
For all groups, the scintimammography true-positive (TP) and false-positive (FP) results were as follows:
- Group 1: 19 TP, 5 FP
- Group 2: 13 TP, 4 FP
- Group 3: 18 TP, 0 FP
- Group 4: 3 TP, 1 FP
Patients in group 3 were being assessed for multicentric disease such as in-situ or lobular carcinoma. Scintimammography accurately diagnosed multicentric lesions, confirmed multicentricity already suspected on traditional workup, and revealed a larger tumor size. The modality did miss one in-situ carcinoma. Lobular carcinoma does pose a diagnostic challenge for traditional imaging, the authors stated.
They acknowledged that the specificity of SM-SPECT was low but attributed that to study design. All radiotracer uptake was considered positive for malignancy and a scoring system was not used, they explained.
Ultimately, scintimammography "diagnosed cancer in 10 cases with a discordant conventional workup (and) ... was found to be decisive in making the diagnosis of cancer in 20 patients with (American College of Radiology) class 3-4 and contradictory FNA results," they wrote.
The next phase in testing the worth of scintimammography would require a prospective study looking at the modality's ability to select patients who should undergo surgery, they added.
In an accompanying JNM commentary, Dr. Orazio Schillaci from the University of Rome Tor Vergata in Italy stated that scintimammography still needed to prove itself against other modalities for picking up on small breast cancers (JNM, October 2005, Vol. 46:10, pp. 1571-1573).
Schillaci said that Mathieu's work substantiated scintimammography as a complementary test, but also advanced its cause by showing that SPECT can improve scintigraphic sensitivity.
"Scintimammography is not the magic bullet for breast cancer," he wrote, "but neither only a false promise."
By Shalmali Pal
AuntMinnie.com staff writer
October 18, 2005
Related Reading
Molecular breast imaging sensitive for detecting smallest tumors, January 1, 2005
Neuroradiotracer may be useful in scintimammography, January 6, 2005
Copyright © 2005 AuntMinnie.com



















