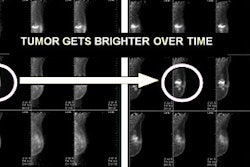
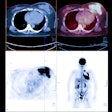
Positron emission mammography (PEM) lends itself to standardized terminology for describing exam results, much like the BI-RADS lexicon for breast MRI. But there are key differences clinicians need to be aware of, advised researchers this month in the American Journal of Roentgenology.
In two papers, lead researcher Dr. Wendie Berg and colleagues sought to define and illustrate standard terminology for describing PEM findings to provide associated rates of malignancy, and to show that multiple readers can interpret with high performance after minimal training (AJR, April 2011, Vol. 196:4, pp. 956-970 and pp. 971-981). At the time of the study, Berg was with the American College of Radiology Imaging Network; she is now with the University of Pittsburgh.
"The overarching goal of both of those studies was to standardize the interpretation of PEM, a task that has to be done with any new technology," Berg told AuntMinnie.com. "We also wanted to demonstrate that multiple readers can interpret images consistently."
Watch 'probably benign'
A multicenter trial comparing PEM to MRI in assessing disease extent included 388 women with newly diagnosed breast cancer who were scheduled to undergo breast-conserving surgery. Berg and colleagues developed terminology to describe PEM findings patterned on BI-RADS for MRI; they also tracked and correlated PEM imaging features of known malignancies and additional PEM lesions.
Berg's group developed a PEM sample feature analysis lexicon that included a seven-point assessment scale:
- 1 = Negative, routine follow-up
- 2 = Benign, routine follow-up
- 3 = Probably benign, short-interval follow-up
- 4a = Low suspicion, biopsy
- 4b = Intermediate suspicion, biopsy
- 4c = Moderate suspicion, biopsy
- 5 = Highly suggestive of malignancy, biopsy
Of 166 additional lesions on PEM, 54 (33%) were malignant, with a median tumor size of 8 mm. Among 43 round or oval masses, 16 (37%) were malignant, compared with 16 (76%) of 21 lobulated or irregular masses.
Berg's group found the following PEM malignancy rates for BI-RADS-like final assessments:
- Category 2: one of 31 (3.2%)
- Category 3: three of 32 (9.4%)
- Category 4a: four of 18 (22%)
- Category 4b: nine of 33 (27%)
- Category 4c: 15 of 24 (63%)
- Category 5: 22 of 28 (79%)
Although most of the malignancies found by PEM matched MRI or mammography results, there were some cancers only PEM identified, Berg and colleagues wrote: Of a total of 116 malignant lesions in 82 breasts identified in the 388 women, 17 (15%) of 116 were found only by PEM.
The study demonstrated that the use of category 3, or "probably benign," is tricky: Three (14%) of 22 contralateral breast lesions categorized this way were malignant, a rate much higher than that expected for lesions recommended for six-month follow-up with other breast imaging modalities.
"We didn't expect this issue with 'probably benign' findings," Berg told AuntMinnie.com. "In breast imaging, a rating of BI-RADS 3 means there's a less than 2% chance of cancer, and the woman can come back in six months for a follow-up. But PEM finds more malignancies, so what you do see, you need to track more aggressively. That's why it's best if facilities that offer PEM also do PEM-guided biopsies."
A matter of training
In the second study, Berg's team trained breast imaging specialists in standardized interpretation of PEM and then validated the performance of these imagers in interpreting MRI. The team found that it didn't take much training for experienced breast specialists to demonstrate high performance in interpreting PEM images.
Berg and colleagues developed a two-hour teaching module to train radiologists to interpret PEM images. The module included a sample feature analysis lexicon analogous to BI-RADS, and 12 sample cases. The radiologists were asked to review 49 PEM images (of which 20, or 41%, were malignant) and 32 MRI images (of which 11, or 34%, were malignant) and assign a feature category. The radiologists did not receive specific training for MRI interpretation, although Berg's team encouraged them to review the BI-RADS lexicon for MRI.
For 36 interpreting radiologists included in the study, mean sensitivity, specificity, and area under the curve (AUC) for PEM were 96%, 84%, and 0.95, respectively. Mean sensitivity, specificity, and AUC for the MRI image interpretations were 82%, 67%, and 0.80, respectively.
Before the tutorial, 32 of the 36 radiologists had reviewed between zero and 20 PEM exams, according to the authors.
"The high diagnostic performance of all 36 observers from 15 different institutions after a two-hour tutorial shows that accurately interpreting PEM images is quickly learned and reproducible for breast imaging radiologists, independent of years of clinical experience," they wrote.
| The studies were funded in part by PET developer Naviscan, which provided the PEM device used. Berg is a consultant with the company. |