While radiation exposure to a fetus from an FDG-PET scan is low, every effort should be made to minimize exposure by modifying the imaging protocol, according to a study in the July issue of the Journal of Nuclear Medicine.
Based on results from five pregnant cancer patients, researchers found fetal radiation exposure to be slightly lower than existing estimates, adding that future studies could provide additional information on how to image this patient population effectively.
The lead author of the study is Dr. Amol Takalkar from the PET Imaging Center at the Biomedical Research Foundation of Northwest Louisiana (JNM, July 2011, Vol. 52:7, pp. 1035-1040).
Balancing risk
The authors cited previous research indicating that cancer occurs in approximately one in 1,000 pregnancies, with malignancies possible in the breast, cervix, thyroid, and ovaries. They noted that pregnant women present a "particularly difficult dilemma," as clinicians weigh the need for imaging against the potential radiation exposure risk to an unborn fetus.
"Lack of accurate, scientific data about the risks and benefits of FDG-PET in diseased pregnant patients combined with medical liability concerns may result in a conservative and potentially inappropriate choice to withhold necessary medical imaging in such situations," Takalkar and colleagues wrote.
The retrospective study enrolled five pregnant patients, ranging in age from 22 to 37 years, who were referred for oncologic FDG-PET scans and had a biopsy-proven diagnosis of cancer. One patient was found to be pregnant a few weeks after her FDG-PET scan; at the time of her FDG-PET imaging, she had a negative urine test for pregnancy.
Two patients had cervical cancer, two had lymphoma, and one had lung cancer.
Because of their pregnancy, the patients received a smaller dose of FDG (173.9 to 340.4 MBq) instead of the standard protocol dose (555 MBq). However, the patient whose pregnancy was discovered after her FDG-PET scan received a dose of 583.12 MBq.
To reduce radiation exposure to the fetus, the PET-only images were acquired in 2D mode (Advance or Discovery LightSpeed 4, GE Healthcare) through an average of five to six five-minute bed positions.
One patient was imaged twice during her pregnancy, at 18 weeks (second trimester) and at 30 weeks (third trimester). Another patient received one FDG-PET scan during her second trimester, and two patients underwent one FDG-PET scan during their third trimester.
Fetal radiation dose was independently assessed for each patient, with researchers manually determining a region of interest over the fetus to help determine dose volume. Total radioactivity in the region was measured on a slice-by-slice basis.
The researchers determined that fetal dose exposure from the FDG-PET scans ranged from 1.1 to 2.43 mGy in the various trimesters of pregnancy. The only exception was the patient in the early stages of pregnancy, whose fetal dose was estimated to be 9.04 mGy.
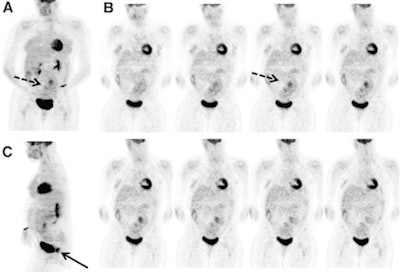 |
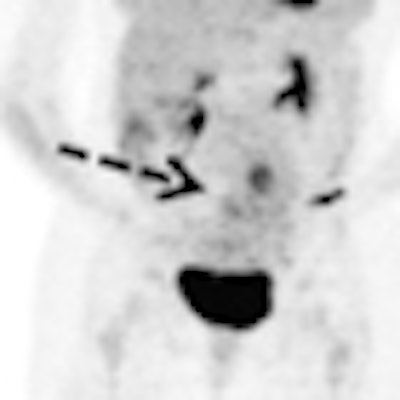
| FDG-PET images are of a 34-year-old woman who was 28 weeks pregnant and diagnosed with squamous cell carcinoma of the cervix. Image (A) shows FDG activity (dashed arrow) related to fetus in pregnant uterus in lower abdomen and pelvis. Two rows of selected coronal images (B) show FDG activity related to fetus in pregnant uterus in lower abdomen and pelvis (arrow). Image in sagittal projection (C) illustrates intense FDG uptake (arrow) in cervical malignancy posterior to urinary bladder activity. Images courtesy of Journal of Nuclear Medicine. |
Most importantly, Takalkar and colleagues found that there was "no prominent focal FDG uptake in other fetal regions in any patient. All patients delivered healthy infants with no visible abnormalities at term."
The group concluded that fetal radiation exposure from FDG-PET scans in pregnant women with cancer is low and "significantly below the threshold dose" to have a definitive effect on the fetus.
"However, all efforts should be made to minimize the fetal radiation exposure by modifying the protocol appropriately," they wrote. "And as more data become available, the current fetal dose estimates may require further modification."




















