Non-small cell lung cancer (NSCLC) patients with negative histologic results and positive mediastinal lymph node findings on preoperative PET scans have a worse prognosis than patients with negative findings, according to a study in the October issue of Radiology.
Based on the findings, researchers from the University of North Carolina (UNC) and Fudan University Shanghai Cancer Center in China concluded that a preoperative PET evaluation of the mediastinum "may complement surgical and histological findings." In addition, the PET-positive results suggest that postoperative radiation therapy and/or chemotherapy may be helpful for these patients.
The lead author of the study is Dr. Liyi Xie from the departments of radiation oncology at both UNC and Fudan (Radiology, October 2011, Vol. 261:1, pp. 226-234).
The researchers reviewed records of patients who underwent surgery for lung cancer at UNC between 2000 and 2006. The 90 subjects enrolled had various stages of NSCLC, were undergoing lobectomy or pneumonectomy, and were not receiving neoadjuvant or adjuvant radiation therapy or neoadjuvant chemotherapy.
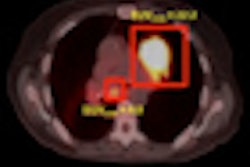
The patients had also received a preoperative evaluation with MRI or CT, and a preoperative PET scan of the chest or whole body. PET/CT scans with FDG were performed with a dedicated PET scanner (Biograph or Biograph 40, Siemens Healthcare). PET images were acquired approximately 60 minutes after the intravenous administration of approximately 444 MBq of FDG, and the images were generally obtained from the base of the brain to the proximal thighs.
All 90 patients had a histologically negative mediastinum, with 44 of the patients having received both mediastinoscopy and surgery. Thirteen patients had positive mediastinal PET findings, whereas 77 had negative findings.
Images from the mediastinum were categorized by two nuclear medicine specialists who evaluated all PET/CT results visually and by standardized uptake values (SUVs). The median follow-up time for all patients was 54.3 months, ranging from one month to 99 months, while the median follow-up time for survivors was 71.7 months, ranging from 47 months to 99 months.
Due to a loss of data, the researchers were able to calculate SUVs for only 48 patients for mediastinal lymph nodes.
Failure rates
Despite negative histologic findings, patients with positive preoperative PET mediastinal lymph node findings had greater five-year rates for both local-regional failure (68%) and distant failure (66%) compared to patients with negative PET findings, who had rates of 19% and 10%, respectively.
These PET-positive patients also had a worse prognosis, with a five-year overall mortality of 77%, compared with 36% for patients with negative PET scans.
Median SUVmax was 2.75, ranging from 1.67 to 5.49, according to the authors. The crude rate of local-regional failure for patients with an SUVmax less than the median was seven of 24, compared with failure of eight of 24 patients with SUVmax greater than the median. The comparable rates of distant failure were four of 24 for those less than the SUVmax median and seven of 24 for those greater than the median.
Surgical complement
The findings suggest that preoperative evaluation of the mediastinum with PET in patients with NSCLC may complement surgical and histologic findings, Xie and colleagues concluded.
"Among patients with a negative pathologic assessment of the mediastinum, those with an abnormality in the mediastinum at PET have a higher rate of local-regional and distant failure than do those without," they wrote. "Thus, positive PET findings in the face of negative histologic findings may represent a false-negative pathologic assessment, rather than a false-positive PET finding."
The high rate of local-regional and distant failure also suggests that postoperative radiation therapy and/or chemotherapy may benefit patients with positive mediastinal findings at preoperative PET, the authors noted.