Optic nerve uptake at baseline on an FDG-PET/CT scan and response after neoadjuvant chemotherapy are strong predictors of event-free and overall survival for young children with stage III retinoblastoma, according to a study in the February issue of the Journal of Nuclear Medicine.
Researchers from the All India Institute of Medical Sciences in New Delhi found that eight, or 32%, of patients in the study with optic nerve FDG uptake on an initial PET/CT scan had lower event-free survival (0%), compared with patients with no optic nerve uptake (60%) at the median follow-up of 15.4 months. Those same eight patients had a lower overall survival rate (14%) than patients with no optic nerve uptake (71%) at median follow-up.
Based on the results, they concluded that FDG-PET/CT could play a role in determining appropriate treatment for these patients before their disease worsens.
Lead study author Dr. Venkatraman Radhakrishnan and colleagues from the departments of medical oncology and nuclear medicine estimated that between 7,000 and 10,000 children in developing countries are diagnosed with stage III retinoblastoma annually, with more than half of them dying from the disease (JNM, February 2012, Vol. 53:2, pp. 191-198).
Currently, CT and MRI of the orbit and brain are the modalities of choice to diagnose and evaluate the extent of retinoblastoma. At the New Delhi facility, all patients with locally advanced retinoblastoma undergo gadolinium-enhanced MRI of the orbit and brain, bone marrow aspiration and biopsy, cerebrospinal fluid examination, and other treatment at the time of retinoblastoma diagnosis.
This study prospectively enrolled 25 stage III patients from the cancer center from May 2009 to June 2010. There were 16 boys and nine girls, with a median age of 3 years, ranging from 2 to 12 years old. The median duration of symptoms before presentation to the facility was six months, ranging from one to 30 months.
Retinoblastoma treatment
Treatment for stage III retinoblastoma included neoadjuvant chemotherapy, removal of the eye, and external-beam radiotherapy and adjuvant chemotherapy. Clinical assessments of treatment response were conducted every four weeks, while gadolinium-enhanced MRI was performed after three cycles of neoadjuvant chemotherapy prior to surgical intervention. Patients also underwent examination under anesthesia of the unaffected eye at baseline and every three months to detect bilateral disease.
Patients in the study were given a median number of 10 chemotherapy cycles, which included neoadjuvant and adjuvant therapy. Eye removal was performed in 20 (80%) of 25 patients, and three patients died before eye removal. Radiotherapy after eye removal was performed on 17 (68%) of the 25 study patients; five patients died before radiotherapy, and three patients were lost to follow-up.
Events were recorded in 13 of 25 patients; eight of 13 patients had central nervous system (CNS) relapse, three had local site progression, and one had local relapse followed by abdominal relapse. Ten of the 25 study patients have died: Nine died because of disease progression and one of an unknown cause.
Whole-body PET/CT scans were performed with a dedicated PET/CT scanner (Biograph 2, Siemens Healthcare) at baseline (PET/CT-1) and after completion of three cycles of neoadjuvant chemotherapy (PET/CT-2). PET/CT-2 was performed after a minimum of four weeks after the third chemotherapy cycle or three to 3.5 months after the start of treatment.
All 25 patients underwent a baseline FDG-PET/CT exam, while 21 of 25 patients underwent postneoadjuvant chemotherapy PET/CT scans. The median follow-up of the study patients was 15.4 months, ranging from 2.2 to 24.3 months.
The event-free survival rate for the participants was 42%, while the overall survival rate was 53% at the median follow-up, according to the authors.
"No significant difference was seen between stage IIIA and stage IIIB patients on PET/CT staging for event-free survival at a median follow-up of 15.4 months" the authors wrote, "However, there was a trend toward better overall survival in patients with stage IIIB than in patients with stage IIIA on PET/CT-1 follow-up of 15.4 months."
Optic nerve uptake
Optic nerve FDG uptake was seen in eight (32%) of 25 patients on the initial PET/CT scan. Those eight patients had a lower event-free survival (0%), compared with patients with no optic nerve uptake (60%) at the median follow-up of 15.4 months. Those same eight patients had a lower overall survival rate (14%) than patients with no optic nerve uptake (71%) at median follow-up.
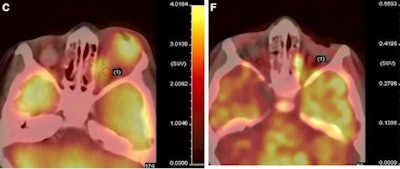 |
| Fused PET/CT images (C) show prosthesis in right eye and large extraocular tumor in left eye, with optic nerve thickening and uptake. After three cycles of neoadjuvant chemotherapy, PET/CT image (F) shows decrease in size of left orbital tumor and optic nerve uptake. Patient died because of brain metastases. Images courtesy of JNM. |
The analysis also showed that eight of the 25 patients developed CNS relapse on follow-up, of which five patients had optic nerve FDG uptake on PET/CT-1.
In addition, the researchers found that event-free survival for patients with complete and partial response to therapy was 62%, compared with 0% for patients whose disease progressed, based on the second PET/CT results at the median follow-up period. Overall survival for patients with complete and partial response to treatment was 69%, compared with 0% for patients with disease progression at median follow-up.
Optic nerve uptake at baseline of PET/CT and response after neoadjuvant chemotherapy was a "strong predictor" of event-free survival and overall survival in stage III retinoblastoma, Radhakrishnan and colleagues concluded. Therefore, PET/CT may play a role in baseline prognostication and response assessment in stage III retinoblastoma.