A coalition of medical societies released new guidelines on dose optimization of cardiac imaging scans on Thursday in the Journal of the American College of Cardiology. The document offers a road map for improving radiation safety and reducing patient radiation dose while obtaining high-quality medical images.
The report is the product of a one-day think-tank meeting held last month to draft a consensus paper that reaches broad conclusions on how to protect patients, assess cancer risk, and guide facilities in developing an action plan for radiation safety.
Meeting participants also laid out plans for developing infrastructure to support "robust dose assessment and longitudinal tracking, collation, dissemination, and implementation of best practices" along with plans for education across the healthcare community and to patients and the public (Journal of the American College of Cardiology, March 20, 2012). The lead author on the paper is Dr. Pamela Douglas, chief of cardiology at Duke University.
Societies participating in the February 28 meeting included the American College of Cardiology Foundation, American College of Radiology, American Heart Association, American Society of Nuclear Cardiology, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, and Society of Nuclear Medicine. However, the document notes that the conclusions it expresses are those of the conference participants only and not of the societies themselves.
Unanswered questions
Advances in medical imaging and growth in procedure volume have resulted in an increase in radiation exposure in cardiovascular patients, and the spike in radiation dose has "rekindled the controversy as to whether the low doses of ionizing radiation used in cardiovascular care may lead to an increased lifetime risk of cancer, and whether such risks can be justified in light of the established medical benefits," the authors wrote.
But despite the increased focus on radiation exposure, many questions remained unanswered.
Addressing the core paradox of all medical radiation exposure, the authors noted that while the use of radiation is undesirable, it is "intrinsic to the current state of the art of cardiovascular care" that has substantially reduced morbidity and mortality from cardiovascular disease (CVD), an outsized killer that is responsible for one of three deaths in the U.S. Thus, the authors said, the goal is to balance the risks and benefits, rather than attempt to eliminate radiation exposure. That means weighing the risks of exposure versus benefits at every step in the process.
"For example, in older patients and those with life-threatening CVDs, the benefits of accurate diagnosis and optimal management that are facilitated by imaging are likely to outweigh the minimal or theoretical risks of optimal radiation exposure," Douglas et al wrote.
Given the difficulty of achieving optimal patient radiation safety in adults, cardiovascular medicine represents a complex and difficult task. The Duke Clinical Research Institute convened the February 2012 think tank to develop practical approaches based on the broadest possible input, the group wrote.
Dosimetry and risk modeling
Addressing the issues of stochastic and deterministic radiation effects, the writing group noted that the "risk and frequency of malignancies caused by the levels of radiation used in medical imaging remains undetermined and controversial."
"However, given this uncertainty, it is critical to educate providers to minimize dose by performing only diagnostic exams and procedures that are appropriate and necessary, considering the benefits and risks of alternative examinations or procedures without radiation, and by using the best possible combination of equipment, dose, and protocols that will still result in accurate and diagnostic studies," they wrote. This is related to the ALARA approach well-known to radiologists -- that of using a radiation dose as low as reasonably achievable (ALARA) to achieve the desired imaging result.
The report addresses the differences between radiation exposure and dose and notes that "the absorbed dose cannot be measured directly but can only be estimated for a given exam, since numerous patient- and exam-specific factors dramatically alter how much radiation is absorbed in different patients for the same imaging protocol from a given device. Thus, even if the scanner-delivered exposure is constant, the number of x-ray photons that reach various tissues and organs varies greatly between individuals."
Modeling risk to patients is equally complex, the group noted, and there are well-known problems with the linear no-threshold (LNT) model, which states that cancer risk increases linearly with dose and that there is no dose level below which there is no risk. The LNT model is frequently challenged by other risk-estimation models.
"Based on the LNT model, the average lifetime risk of cancer mortality in the general population attributable to an effective dose of 1,000 mSv (an exposure equal to 50 to 500 typical coronary CT angiograms or radionuclide perfusion studies) is estimated at 5% to 7.9%," the group wrote. "However, prospective, long-term observational studies have not unequivocally confirmed an increased risk of solid cancers related to medical or occupational low-dose radiation (< 100 mSv) delivered over many years, thereby neither confirming nor refuting the LNT model."
Estimation is complicated by the low doses in medical exams and by the long latency period for the development of most cancers.
Toward protecting patients
"Approaches to patient radiation safety must be lifelong and not confined to simply reducing the exposure during a single test or procedure," the authors stated. For this reason the American College of Radiology (ACR) and the National Council on Radiation Protection and Measurements (NCRP) suggest that radiation reduction efforts be divided into those that occur before, during, and after an imaging procedure to ensure lifelong safety. That means planning before exams are undertaken.
"Tests and procedures utilizing radiation should be performed in the right patient, for the right reason, at the right time, and alternatives to radiation should be considered," they wrote. For appropriateness, the American College of Cardiology Foundation (ACCF) appropriate use criteria "offer an important framework to ensure appropriate use," they wrote. In addition, the International Commission on Radiological Protection (ICRP) and American Heart Association have developed reference levels for use as benchmarking and quality-assurance tools, the authors noted.
The enormous variation in radiation dose for all types of imaging procedures within and across institutions for coronary CTA and nuclear medicine procedures is evidence of the need for increased standardization. Professional organizations have developed thorough safety and procedure guidelines to address these issues, the authors noted.
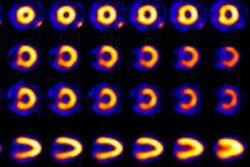
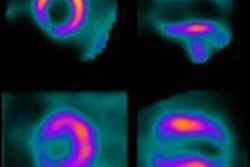
Technology has enabled dramatic dose reductions for CCTA (i.e., prospective triggering) and nuclear imaging (i.e., the use of technetium instead of thallium) and promises additional dose-reduction techniques in the future. Scanners increasingly capable of providing real-time readouts of dose estimates can be used for benchmarking, quality improvement, research, and equipment operation.
After imaging, the focus should shift to tracking and reporting doses, particularly to track exposure and avoid excessive cumulative radiation doses for individual patients. This process is fraught with uncertainty for several reasons, including the "inherently random nature of stochastic events," and because exposure tracking is difficult to perform accurately and "has no clear value for improving long-term patient safety," they noted. An important exception is the tracking of high-dose events, such as percutaneous coronary interventions, ablation procedures for cardiac arrythmias, and the use of high-dose fluoroscopic procedures.
Developing an action plan
The uncertainty surrounding dose and patient care issues requires the input and expertise of many stakeholders. Critical areas for action developed include quantifying the estimated stochastic risks of low-dose radiation associated with cardiovascular imaging and therapeutic procedures.
In addition, research is needed to evaluate biological markers of cellular radiation injury as predictors of radiation-induced cancer, determine the dose-response relationship between radiation and molecular and cellular effects, and improve techniques for modeling and simulation to estimate radiation dose, they wrote.
The authors cited the need to encourage basic and translational research related to mechanisms by which "radiation-induced cellular DNA damage and cellular repair and misrepair mechanisms affect radiation-related carcinogenesis," they wrote. Important areas of research include biological markers of injury, models of injury, and improvement of techniques for modeling and simulation of these effects, as well as on true long-term risks of exposure.
Measuring and developing the ability to more accurately track dose in multiple settings should also be a priority, as "rigorous radiation dose estimates are typically obtained only in specific situations, when detailed dosimetry is required," the group wrote.
Tracking dose should include the establishment and implementation of standards to ensure consistent recording of radiation exposure and patient parameters needed to estimate dose, and expansion and development of central registries related to radiation exposure and cardiovascular imaging to support best practices and new research. The authors specifically called for an automated, multispecialty national dose registry.
Standards are also needed for communicating radiation exposure within the healthcare community. As they are being developed by multiple stakeholders, available measures of exposure, such as dose-area product, should be documented and reported in clinical studies. A standard vocabulary should eventually be introduced to reduce the use of jargon and conflicting language, and, once developed, its use should be mandatory, they wrote.
Strategies are also needed to minimize radiation dose from single episodes of care. Gaps in provider knowledge, differences in image-acquisition protocols, and limited transparency lead to delays and fragmentation in the implementation of known dose-reduction opportunities, the authors wrote.
The lack of incentives to minimize dose and engrained practice routines based on defensive medicine may hinder the adoption of appropriate imaging use, but application of existing American College of Cardiology Foundation appropriate-use criteria could go a long way toward reducing these barriers, the authors noted.
"Tools in development include multimodality appropriate use criteria, which will simultaneously assess the appropriateness of testing alternatives in specific clinical scenarios, including methods that do not involve ionizing radiation and imaging performance measures," Douglas et al wrote. "To fully implement any of these, the healthcare system should develop incentives for their use."
Opportunities to reduce variability in the performance of image-guided procedures include patient shielding "during fluoroscopic procedures, reduction of fluoroscopy and cineangiography procedural times, and image processing techniques to eliminate unnecessary duplicated images and radiation exposure," they wrote.
Radionuclide dose-reduction techniques include the use of stress-only imaging, PET, and adoption of new camera technology that provides for dramatic reductions in dose. In addition, technological developments will lead to new opportunities for dose reduction, but it's important to avoid "overly proprietary techniques," the group noted.
Finally, "sustained education and quality improvement programs can lead to meaningful radiation dose reduction," they wrote. Such programs should recognize the opportunity to engage not only imagers, but also physicians who order imaging tests.
Although it is impossible to completely assess the risk-benefit relationship without additional research, efforts to apply the basic principles of radiation protection and facility-level tracking are "eminently feasible," the group wrote.
"Although safety is always paramount, consideration of the benefits as well as the risks of medical tests and procedures is in the patient's best interest, as is the use of sufficient radiation to ensure diagnostic or therapeutic success," Douglas et al wrote. "Attention must be paid to optimizing patient care and not merely technical information."