Results from a randomized clinical trial being presented at this week's American Academy of Neurology (AAN) meeting suggest that the SPECT radiopharmaceutical DaTscan (ioflupane I-123 injection) can help clinicians distinguish between tremors due to Parkinson's disease and nonparkinsonian essential tremor, expediting appropriate treatment.
Among patients imaged with the agent, 54% had a change in diagnosis within one year from general neurologists and movement-disorder specialists, compared with a 23% changed-diagnosis rate in patients not imaged using the agent (p < 0.001). Furthermore, 41% of DaTscan subjects had changes in clinical management during the year of follow-up, compared with 22% of those in the control group (p < 0.001).
The results were presented today at the AAN meeting by Dr. Igor Grachev, PhD, global head of DaTscan in the medical affairs division at GE Healthcare. The study was conducted by seven general neurologists and 12 movement-disorder specialists; results were also published online on April 6 in the Journal of Neurology, Neurosurgery, and Psychiatry.
Multicenter trial tackles tracer's efficacy
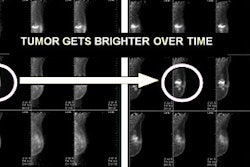
DaTscan was approved by the U. S. Food and Drug Administration (FDA) in June 2011 for striatal dopamine transporter visualization using SPECT imaging as an adjunct for evaluating adults with suspected parkinsonian syndromes (PS). A team conducted a 19-center trial in the U.S. and Europe to bolster previous nonrandomized or retrospective studies indicating that the tracer helps to confirm suspected parkinsonian syndromes (Movement Disorders, October 2004, Vol. 19:10, pp. 1175-1182; European Journal of Nuclear Medicine and Molecular Imaging, July 2008, Vol. 35:7, pp. 1367-1376).
A total of 259 patients were included in the safety portion of the study. They had experienced symptom onset in the previous five years, and they had a diagnosis of clinically uncertain parkinsonian syndrome or monosymptomatic, atypical, or incomplete presentation of parkinsonian signs and symptoms. Fifteen of these patients were excluded.
A subset of the total population consisting of 215 patients was examined, representing all subjects who had the full set of four follow-up visits and who were analyzed to see whether DaTscan use led to a change in clinical diagnosis over one year.
At one year, 54% (55 of 102) of the DaTscan subjects had a change in diagnosis, compared with 23% (26 of 113) of the controls (p < 0.001). There also was a significantly greater mean change from baseline in confidence of diagnosis for DaTscan patients compared to controls at one year.
The most common change in management was initiation of medication not planned at baseline, including initiation of dopaminergic therapy, according to the researchers.
There was not a statistically significant difference between the two physician groups in change in clinical management of all the patients over the year. However, 75% of DaTscan patients treated by neurologists had a change in diagnosis, compared with 47% of those treated by a movement-disorder specialist (p = 0.022).
"These data show DaTscan is useful for both general neurologists and movement-disorder specialists," said Grachev.
The researchers also used the Parkinson's Disease Questionnaire (PDQ-39) to analyze health status and the EQ-5D quality-of-life questionnaire. They did not find any significant improvements in scores in the DaTscan group compared to controls.
Grachev said this may be because patients were at the early stage of disease.
"Also, it could be because these scales were developed for Parkinson's disease, not for [clinically uncertain parkinsonian syndromes (CUPS)]," he said. "So we still don't know how sensitive these assessment measures are for detecting changes in CUPS patients."