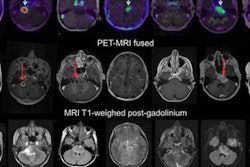
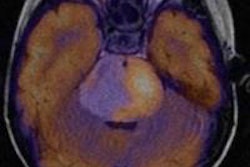
MIAMI BEACH, FL - In cases of single-tumor lesions in pediatric patients, combined PET/MRI proved most beneficial for tumor staging, while both modalities alone outperformed each other in different diagnostic situations, according to a study presented on Monday at the Society of Nuclear Medicine (SNM) meeting.
Researchers from the University of Munich found that MRI alone was superior to FDG-PET and software-registered FDG-PET/MRI for primary diagnosis, but FDG-PET alone was better than MRI alone in the follow-up exams.
"MRI is recommended as the method of choice during primary diagnosis and should be complemented by FDG-PET in cases of unclear multifocal disease," said study co-author Dr. Thomas Pfluger from the university's department of nuclear medicine. "For follow up, FDG-PET is the most effective [modality]."
In the study, led by Dr. Henriette Melzer, also from the university's department of nuclear medicine, the researchers first conducted a separate image analysis with each modality, followed by an analysis of combined registered PET and MR images from each standalone device. The standard of reference was histopathology and imaging follow-up.
A total of 270 FDG-PET and 270 MRI examinations (with a mean interval of five days) were performed on 132 patients. Images were acquired on separate scanners, and hybrid PET/MRI images were produced via software registration.
Of the total patient population, 117 had proven malignant disease and 15 had suspected malignant disease. There also were 64 patients with solid tumors, 53 with systemic malignancy, and 15 with benign disease.
The researchers analyzed 259 suspected tumor lesions during primary diagnosis and 554 lesions at follow-up. All 813 lesions were evaluated and confirmed through histopathology (158 lesions) and/or imaging follow-up (655 lesions) after six months.
When analyzing the results on a per-lesion basis, FDG-PET achieved sensitivity of 86%, compared with sensitivity of 94% for MRI. Specificity for FDG-PET was 85%, but MRI had considerably lower specificity at 38% due to a high number of false-positive findings.
There were discrepant findings for 326 lesions. When the two modalities were combined to classify those abnormalities, sensitivity increased to 97%, but the specificity for FDG-PET (81%) was not raised significantly.
Why so many false positives?
There were 69 false-positive results with FDG-PET, compared with 281 false-positive findings with MRI and 80 with combined FDG-PET/MR images.
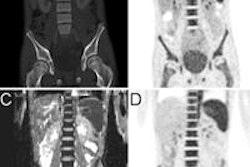
Pfluger attributed FDG-PET's false-positive findings to inflammatory tissues, which accumulate the radiotracer, and post-therapeutic changes in FDG-PET images. False-positive MRI results were triggered by persistent bone marrow edema.
There were false-negative results for FDG-PET in 50 cases, compared with 20 for MRI. Pfluger said false-negative FDG-PET cases were due to small residual lesions and, more importantly, the physiological uptake in the urinary tract, which can obscure tumor lesions. False-negative MRI findings were caused by relatively small soft-tissue changes.
When analyzing results on a per-exam basis during follow-up, sensitivity and specificity were similar. Sensitivity for FDG-PET was 91%, compared with MRI at 93%. FDG-PET reached specificity of 81%, compared with 30% for MRI. Combined FDG-PET/MRI with image registration achieved sensitivity of 96% and specificity of 72%.
'Unacceptable' results
"During follow-up time, specificity of MR alone is unacceptable due to the persistent bone marrow lesions," Pfluger added.
The researchers concluded that on a lesion-based evaluation, combined FDG-PET/MRI with image registration is the best choice for detecting single-tumor lesions and for adequate tumor staging.
"When looking at the examination-based evaluation, which is clinically more important, MR is superior to FDG-PET and combined imaging," Pfluger said. "MR is necessary in any case for exact intervention plans. That is the most important point -- that we need MR for operative biopsy planning."
On the other hand, he added, in follow-up situations, based on the examination-based evaluation, the specificity of MRI is "unacceptable due to the persistent bone marrow edema."