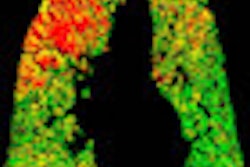
In vivo ventilation/perfusion (V/Q) SPECT imaging can detect early changes to lungs caused by cigarette smoke exposure and provides a noninvasive method for studying lung dysfunction in preclinical models, concluded a study published in the April issue of the Journal of Nuclear Medicine.
These results can be applied clinically to study and diagnose the early stages of chronic obstructive pulmonary disease (COPD), according to researchers from McMaster University and the Firestone Institute for Respiratory Health at St. Joseph's Healthcare in Hamilton, Ontario.
The preclinical study results suggest that V/Q SPECT imaging can detect early and small changes in lung pathology and provide insight into underlying pathologies, which current measures of lung function cannot do, said study co-author Renée Labiris, PhD, in a statement.
In the study, groups of mice were exposed to cigarette smoke for 50 minutes twice daily, five days a week, for either eight or 24 weeks. Age-matched control groups of mice were also included in the study for comparison.
After the final cigarette smoke exposure, V/Q SPECT was performed, followed by a CT scan. Histologic lung sections were then collected and a semiautomated quantitative analysis of airspace enlargement was applied to whole histology slices.
Labiris and colleagues found functional impairment in the lungs due to increased inflammation and airspace enlargement. This impairment, measured with SPECT V/Q imaging, identified COPD characteristics before CT detected structural changes in the lungs, the group found.
The imaging technology used in the study can be conducted in both preclinical and clinical settings, enabling researchers to translate preclinical investigations of disease, associated functional abnormalities, and future drug targets to better understand and manage COPD, according to Labiris.