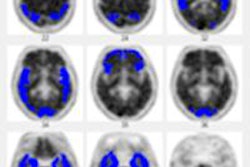
A review of clinical studies on the efficacy of beta-amyloid PET for Alzheimer's disease has led the Institute for Clinical and Economic Review (ICER) to conclude that evidence supporting the scans is still lacking, according to an article published online September 30 in JAMA Internal Medicine.
The ICER piece coincidentally comes three days after the U.S. Centers for Medicare and Medicaid Services (CMS) issued a final decision upholding its July position. CMS confirmed its belief that there is not enough evidence to conclude that beta-amyloid PET is "reasonable and necessary" for diagnosing or treating dementia or neurodegenerative disease.
Lead author Dr. Steven Pearson, ICER founder and president, and colleagues wrote there are "extremely limited data" to demonstrate beta-amyloid PET's utility.
"There are reasonable data showing that, when read by well-trained interpreters, [beta-amyloid PET] is highly accurate in determining whether there is amyloid in the brain," they continued. "However, the clinical utility of a positive scan result remains uncertain," and more studies are needed (JAMA Intern Med, September 30, 2013).
Study review
Pearson and colleagues reviewed 15 studies: One assessed the effect of beta-amyloid PET on diagnostic impression, while 14 evaluated its diagnostic accuracy. Of these 14 studies, 13 compared imaging results with clinical diagnoses or with Alzheimer's diagnosed by biopsy. No studies evaluated diagnostic action, according to the authors.
Among the research cited was a 2009 study from the Mayo Clinic, which found that approximately one-third of cognitively normal older adults would test positive for brain amyloid on a PET scan (Brain, May 2009, Vol. 132:5, pp. 1355-1365). This indicates that a positive beta-amyloid PET result is not diagnostic of Alzheimer's, Pearson and colleagues wrote.
More recently, in the study evaluating diagnostic impression, 229 subjects with progressive cognitive decline and suspected Alzheimer's were examined to determine the potential impact of beta-amyloid PET on diagnosis and treatment management (Alzheimer Disease & Associated Disorders, January-March 2013, Vol. 27:1, pp. 4-15).
The results from 113 positive and 116 negative scans led to a change in reported diagnosis for 55% of cases, with a change in at least one facet of intended management in more than 85%. A limitation of the study, however, was the measurement of "intended" rather than "actual" changes.
Another study analyzed beta-amyloid PET's ability to provide information on whether study participants would progress from mild cognitive impairment to full dementia (Neurology, October 2012, Vol. 79:16, pp. 1636-1644).
Among older participants with mild cognitive impairment, 29% with a positive scan developed full dementia within 18 months, compared with 10% with a negative scan. "However, the data were insufficient to predict whether, or when, cognitive deterioration would occur in individuals with positive scan results," Pearson and colleagues wrote.
Limited effectiveness
Given the limited effectiveness of currently available Alzheimer's treatments, data demonstrating that beta-amyloid PET "leads to changes in clinical impressions and intended management is insufficient," the authors concluded. "More persuasive evidence that [beta-amyloid] PET improves patient outcomes is needed."
In an editorial also published online September 30 in the journal, Dr. Robert Steinbrook, an adjunct professor of medicine at Dartmouth Medical School, concurred with Pearson et al, writing that the "evidence tells us that the role of these scans is uncertain in many situations ... for example, if a positive scan result leads to labeling a person as having a dread and incurable disease and that potential diagnosis turns out to be wrong."
"CMS has proposed a courageous and innovative approach -- to pay for [beta-amyloid] PET as part of coverage with evidence development," allowing meaningful data to be gathered, Steinbrook wrote.
"It would be irresponsible for the CMS to cover [beta-amyloid] PET imaging without adequate evidence about its role in [Alzheimer's] or other neurodegenerative diseases," he added.