CHICAGO - New York researchers have found that radioimmunotherapy (RIT) offers a strategy for curing human immunodeficiency virus (HIV) infection, according to a study highlighted on Tuesday at the RSNA 2013 meeting.
Highly active antiretroviral therapy (ART) keeps the number of viral particles in a patient's bloodstream very low, greatly improving the prognosis for those infected with HIV. But despite the therapy's success in reducing the burden of HIV in the body, dormant infected cells remain, blocking the possibility of a permanent cure.
Lead author Ekaterina Dadachova, PhD, of Albert Einstein College of Medicine, and colleagues investigated whether radioimmunotherapy could destroy remaining HIV-infected cells in blood samples of patients treated with antiretroviral therapy. The team applied radioimmunotherapy to blood samples from 15 HIV patients treated with highly active antiretroviral therapy at the Einstein-Montefiore Center for AIDS Research.
 Ekaterina Dadachova, PhD, from Albert Einstein College of Medicine.
Ekaterina Dadachova, PhD, from Albert Einstein College of Medicine.
"Antiretroviral therapy makes AIDS a chronic disease," Dadachova said. "But people are still dying from AIDS. We need a strategy for eradicating HIV, blocking infection of new cells, and eliminating existing infected cells. Our study addressed the question of whether ART and RIT can work in concert to eradicate HIV-infected human cells."
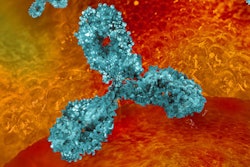
Radioimmunotherapy has historically been used to treat cancer. It uses monoclonal antibodies -- cells the immune system recruits to identify and neutralize antigens -- designed to recognize and bind to specific cell antigens. The antibodies are paired with a radioactive isotope; when injected into the patient's bloodstream, they travel to the target cell and deliver the radiation. Dadachova's team paired the monoclonal antibody mAb2556, designed to target a protein on the surface of HIV-infected cells, with the radionuclide bismuth-213.
"RIT is a nuclear medicine technique developed for cancer treatment, and we're translating it into the field of infectious disease," Dadachova said. "And it's available in tertiary centers; it doesn't require any special suites and can be performed on an outpatient basis."
The study demonstrated that a 4 microcurie (µCi) dose of bismuth-213 killed more than 80% of HIV-infected lymphocytes that had been previously treated with antiretroviral therapy -- reducing the HIV infection in the blood samples to undetectable levels, Dadachova said.
"Our patients were responsive to RIT regardless of time since infection," she said. "We had some patients who had been infected 20 years before, and some that had been infected for a year, but both types responded."
A key finding of the study was that the radiolabeled antibody crossed the blood-brain barrier and destroyed HIV-infected cells without any overt damage to the barrier itself, Dadachova said. Antiretroviral treatment only partially penetrates this barrier, which means that even if a patient's system is free of HIV, the virus continues to damage the brain, causing cognitive disorders and mental decline.
"Many patients on antiretroviral therapy suffer from HIV-associated neurocognitive disorders as the brain becomes a reservoir for infection," Dadachova said. "Our study found that RIT does not disrupt the blood-brain barrier, which is important for our patients."
Going forward, Dadachova's team plans to investigate the ability of RIT to kill latently infected cells in patients who are not on ART.
"We're preparing a clinical trial for 2014 in ART-naive HIV patients in collaboration with the University of Pretoria in South Africa, and hope to have results by the end of the year," she said.