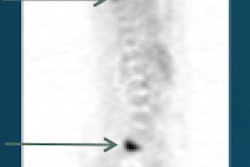
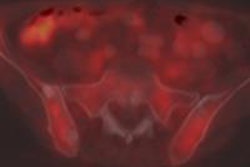
Whole-body metabolic tumor volume, as determined by FDG-PET/CT before treatment, is a reliable prognosticator of overall survival in patients who have invasive ductal carcinoma (IDC) of the breast and distant metastases at the time of their initial diagnosis, according to a study published online July 23 in the American Journal of Roentgenology.
The researchers from Korea also found that determining the maximum standardized uptake value (SUVmax) of whole malignant lesions and whole-body total lesion glycolysis are useful in predicting overall survival for these patients.
In addition, the "presence of visceral metastasis was significantly associated with a worse prognosis, although this result was not confirmed by multivariate analysis," wrote the group, which was led by Dr. Seung Hyun Son from Kyungpook National University Medical Center and School of Medicine.
Predicting survival time
Research has shown that survival time for patients with invasive ductal carcinoma and metastases varies significantly, from less than nine months to more than three years, the authors noted.
SUVmax has been regarded as a prime indicator of survival; however, if only the lesion with the highest SUVmax is evaluated in patients with metastatic disease, this may underestimate the risk from other metastatic sites.
"Accordingly, we considered that whole-body metabolic tumor volume would better reflect disease status and, thus, better predict prognosis in patients with metastatic breast cancer," they wrote. "To our knowledge, this is the first study that has used whole-body metabolic tumor volume as a predictor of prognosis for patients with metastatic breast cancer" (AJR, July 23, 2015).
Son and colleagues enrolled 40 patients who underwent FDG-PET/CT between January 2006 and December 2011 to stage their primary IDC before treatment. The women had a mean age of 49.1 years (range, 29-75 years).
The patients received approximately 8.1 MBq of FDG per kilogram of body weight. The mean time from diagnosis of breast cancer to the FDG-PET/CT scan was 4.3 days. All 40 subjects also underwent mammography, sonography, bone scans, breast MRI, and conventional contrast-enhanced CT for pretreatment clinical staging.
All of the women were treated with chemotherapy, hormone therapy, or both in the first round of treatment. Radiation therapy was performed concurrently with systemic chemotherapy or hormone therapy for 31 women, and 15 of the 40 patients underwent palliative surgery in their second round of treatment.
The researchers manually designated a region of interest (ROI) to include the primary tumor or metastatic lymph nodes or distant metastatic sites, and SUVmax was calculated. Overall survival time was defined as the date the FDG-PET/CT scan was conducted to the date of a patient's death. For survivors, the last follow-up examination in December 2013 was used as the end point.
Cutoff values
Among the 40 patients, 21 (52%) died during the mean follow-up period of 36.4 months (range, 0.8-71.4 months).
Analyzing the area under the receiver operator characteristics (ROC) curve, Son and colleagues determined an optimal cutoff value of 167.8 cm3 for predicting overall survival using whole-body metabolic tumor volume.
Median overall survival was 19.7 months in patients with whole-body metabolic tumor volume greater than 167.8 cm3, with 10 deaths among this group. Meanwhile, in those with volume less than 167.8 cm3, survival time was 68 months, with 11 deaths.
| Survival by parameter cutoff values | |||||
| No. of patients | No. of deaths | Median overall survival (months) | |||
| SUVmax of whole malignant lesions | |||||
| Less than 13.6 | 33 | 15 | 48.5 | ||
| More than 13.6 | 7 | 6 | 21.3 | ||
| Whole-body metabolic tumor volume | |||||
| Less than 167.8 cm3 | 28 | 11 | 68.0 | ||
| More than 167.8 cm3 | 12 | 10 | 19.7 | ||
| Whole-body total lesion glycolysis | |||||
| Less than 194.2 | 15 | 5 | 68.0 | ||
| More than 194.2 | 25 | 15 | 36.8 | ||
The researchers also determined cutoff values for the highest SUVmax of whole malignant lesions and for whole-body total lesion glycolysis.
At a cutoff of 13.6 for SUVmax, those above had a median overall survival of 21.3 months, with six deaths. Subjects under that cutoff point had a median overall survival of 48.5 months, but there were 15 deaths in this group.
For whole-body total lesion glycolysis, women above the cutoff of 194.2 had a median overall survival of 36.8 months, with 15 deaths in this group. Subjects below the cutoff had a median overall survival of 68 months, with only five deaths in this group.
Insufficient parameters
Son and colleagues also tested several other parameters to determine their influence in determining overall survival. Age, nodal stage, triple-negative breast cancer status, hormone receptor status, SUVmax of the primary tumor, and axillary lymph node SUVmax did not help predict overall survival.
Their univariate analysis did identify tumor category, the performance of palliative surgery, and the presence of visceral metastasis as prognostic factors, in addition to SUVmax of whole malignant lesions, whole-body metabolic tumor volume, and whole-body total lesion glycolysis.
Women who received palliative surgery generally had better outcomes than patients who were treated without surgery. While it is "not clear whether performing surgery affects outcome or whether patients who undergo palliative surgery generally have a longer life expectancy and better overall health," it's possible that both aspects could influence outcome for these women, the authors wrote.
However, of all the parameters, only whole-body metabolic tumor volume independently predicted overall survival on multivariate analysis, they concluded.
Son and colleagues cited several limitations to the study, including its retrospective approach and small patient sample, along with differences in the timing of follow-up imaging and patients' treatment regimens.
"The results of the current study need to be confirmed in a larger cohort of patients who have more homogeneous characteristics," they added.