Perfusion imaging with PET/MRI could offer a "comprehensive myocardial ischemic evaluation" with shorter scan times than SPECT and a lower radiation dose for patients, according to a pilot study from Washington University and Barnes-Jewish Hospital in St. Louis.
Researchers used simultaneous nitrogen-13 (N-13) ammonia PET imaging and gadolinium-based MRI to achieve sensitivity and negative predictive values of 100% among patients with positive gated SPECT results.
The hybrid imaging technique offers a "shortened stress perfusion examination and abbreviated protocol with a full study lasting less than 30 minutes of exam time," said lead author and cardiologist Dr. Amir Durrani. "This would then lead to less radiation exposure for patients with no second dose of N-13 ammonia being administered and MRI used to assess liability, as opposed to FDG."
Ammonia-PET for stress perfusion
Previous studies have confirmed the efficacy of pharmacologic stress perfusion imaging with N-13 ammonia PET and contrast-enhanced MRI to detect coronary artery disease. Given those findings, the researchers hypothesized that simultaneous PET/MRI could be extended to cardiac perfusion imaging and identifying coronary artery disease.
"We set out to demonstrate the feasibility of nitrogen-13 ammonia PET/MRI stress myocardial perfusion imaging and determine the accuracy from an abbreviated stress-only PET/MRI exam alongside late gadolinium enhancement, compared to the full exam," Durrani said in his presentation of the pilot study at RSNA 2015.
The researchers identified 16 patients who had positive gated SPECT myocardial perfusion imaging scans. Results were deemed positive if the patient had a reversible myocardial perfusion defect in at least two of 17 contiguous wall segments.
"Based on this positive test, these patients had been scheduled for coronary angiography, which served as the reference standard," Durrani told RSNA attendees.
The nine women and seven men had an average age of 55 years and weighed approximately 80 kg (176 lb). A dozen patients were hypertensive and four patients were diabetic.
The researchers then developed an optimized protocol for a comprehensive cardiac N-13 ammonia PET/MRI scan to evaluate the hybrid modality's diagnostic accuracy for coronary artery disease, compared with gated SPECT myocardial perfusion imaging.
"The primary outcome that we examined, as a comparison of diagnostic accuracy of each imaging modality, was to detect coronary artery stenosis greater or equal to 50%," Durrani said.
The patients were asked to fast overnight and received 400 micrograms of the vasodilator regadenoson as part of the pharmacological stress test. Thirty seconds later, they were simultaneously given N-13 ammonia (10.2 ± 0.46 mCi) for the PET scan and gadolinium-based contrast (0.075 mmol/kg) for MRI perfusion imaging.
The procedure was repeated at rest with a 50-minute delay between rest and stress imaging. PET images were acquired for 15 minutes during both the rest and stress phases, during which MRI stress perfusion took 90 seconds.
MR images were electrocardiogram-gated, and the researchers used a dual-echo volumetric interpolated breath-hold examination (VIBE) Dixon sequence for PET attenuation correction.
Modality comparisons
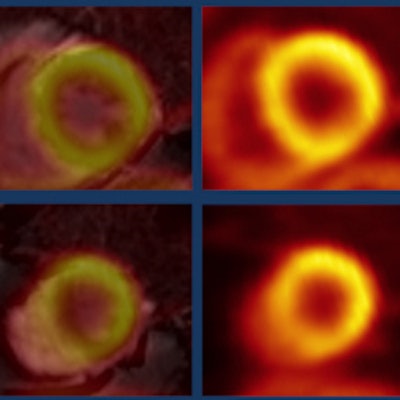
Of the 16 patients in the pilot study, 14 completed both the stress and rest phases of the procedure. Two independent readers evaluated the results by assessing the presence and absence of ischemia and infarction. Areas of decreased perfusion on MRI were correlated with PET myocardial blood flow.
PET/MRI achieved excellent agreement with coronary angiography results and reached greater diagnostic accuracy (64%) than gated SPECT (50%), the researchers found. For coronary artery disease, PET/MRI registered sensitivity and a negative predictive value of 100%, "indicating the potential for a powerful study," Durrani said.
Positive predictive value, however, was only 58%, and specificity was 29%. Durrani suggested that the lower results were "affected by our knowledge and the readers' knowledge that we were recruiting patients who were known to have positive gated SPECT studies. So [readers] were operating on the higher end of the [receiver operator characteristics (ROC)] curve when they read the PET/MRI exams."
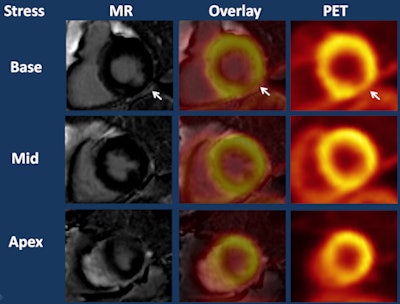 Late gadolinium enhancement images (left column) show infarction in the inferolateral wall (arrow) and PET stress perfusion images (right column) show hypoperfusion in the same region (arrow) that was slightly larger than the infarct. PET/MRI (middle column) indicates mixed infarct/ischemia. Image courtesy of Dr. Amir Durrani.
Late gadolinium enhancement images (left column) show infarction in the inferolateral wall (arrow) and PET stress perfusion images (right column) show hypoperfusion in the same region (arrow) that was slightly larger than the infarct. PET/MRI (middle column) indicates mixed infarct/ischemia. Image courtesy of Dr. Amir Durrani.Abbreviated protocol
With the knowledge that PET has greater sensitivity for identifying ischemia and that late gadolinium enhancement aids in discovering infarcts, the researchers then investigated an abbreviated protocol that eliminated the rest phase of the procedure, and analyzed its effect on sensitivity, specificity, and predictive values.
Analysis of results from the shortened exam showed that sensitivities and negative predictive values remained the same, "preserved across both the abbreviated and the full protocols," Durrani said. "Once again, specificity and positive predictive value suffered for the aforementioned reasons."
More importantly, diagnostic accuracy remained the same for PET/MRI with the abbreviated protocol, at 64%, compared with 50% for SPECT, he added.
"The benefits of simultaneous PET/MRI myocardial perfusion imaging are potentially more accurate [results] than gated SPECT stress in this small-sample-size study, and the abbreviated PET/MRI exam has diagnostic accuracy comparable to the full stress and rest exam," Durrani concluded.
Given the almost identical results, the researchers suggested that the shortened stress perfusion scan and abbreviated protocol could become a full study of fewer than 30 minutes.
"This would then lead to less radiation exposure for patients with no second dose of N-13 ammonia being administered and MRI used to assess liability, as opposed to FDG," he added. "Basically, we would use the stress phase and the late gadolinium enhancement component to potentially replace the rest phrase."
Durrani and colleagues plan to refine the protocols for other potential studies, based on the data presented at RSNA.
"Also, we will increase our sample size in the coming months," he said.