The combination of FDG-PET and MR enterography can accurately differentiate fibrotic strictures and inflammation in patients with Crohn's disease, potentially helping patients avoid unnecessary surgery, according to a new study published in the March issue of Radiology.
In a small preliminary study, researchers from Italy and Massachusetts General Hospital found that a combination of maximum standard update values (SUVmax), signal intensity on T2-weighted MR images, and apparent diffusion coefficient (ADC) values were the most effective biomarkers in distinguishing between patients with fibrosis and cases of fibrosis with active inflammation. The ultimate benefit for patients, the authors concluded, is that PET/MR enterography may have a "potential role" in distinguishing between patients who will need surgery and those who could be treated with noninvasive therapy.
"Importantly, our data suggest that a hybrid biomarker that incorporates both MR imaging and PET information performs better in stricture evaluation than either modality does alone," added lead author Dr. Onofrio Catalano, from the University of Naples "Parthenope" in Italy, and colleagues (Radiology, March 2016, Vol. 278:3, pp.792-800).
Imaging's limitations
While imaging plays a key role in assessing the extent of Crohn's disease and related fibrotic strictures, inflammation, and obstructions in any part of the gastrointestinal tract, the authors noted that CT enterography, MR enterography, and PET/CT have had limited success in detecting intestinal fibrosis, because the fibrosis is "often masked by concomitant active inflammation."
Catalano and colleagues hypothesized that the combination of FDG-PET to provide metabolic information and MRI to gather anatomic detail and soft-tissue contrast could make the hybrid modality useful for evaluating Crohn's disease, "specifically its ability to help distinguish inflammatory from fibrotic strictures."
In this study, 19 consecutively recruited patients received PET/MR enterography for Crohn's disease from December 2012 to October 2014 and underwent bowel resection within five weeks of imaging. The cohort included 13 women and six men (mean age of 37 years ± 13 years) and 33 bowel segments (10 colic, 11 ileal, and 12 ileocolic) with matching PET/MR enterography and histologic findings.
Images from PET/MR enterography (Biograph mMR, Siemens Healthcare) were acquired with the addition of two 12-channel body coils, which were combined to create a multichannel abdominal and pelvic coil. PET/MR enterography began approximately 80 minutes (± 12 minutes) after FDG injection.
Researchers designated regions of interest after bowel segment locations were identified and matching T2-weighted diffusion-weighted MR images, ADC maps, and PET standardized uptake values maps were placed over the entire bowel wall. Signal intensity on T2-weighted images, ADC values, and SUVmax values then were recorded for each bowel segment.
Best biomarkers
The analysis of images and biomarkers found that SUVmax, signal intensity on T2-weighted images times SUVmax, and ADC times SUVmax were the most effective methods in differentiating between patients with fibrosis, cases of fibrosis with active inflammation, and active inflammation only.
More specifically, the best method of determining that difference was the combined PET/MR enterography biomarker ADC times SUVmax cutoff of less than 3,000. The calculation resulted in a mean sensitivity of 67%, a mean specificity of 73%, and a mean accuracy of 71%.
The second-best differentiator was PET SUVmax of less than 2.5, which achieved a mean sensitivity of 79%, mean specificity of 61%, and mean accuracy of 67%. The difference in accuracy between the two methods was statistically significant.
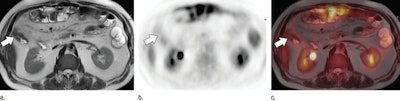
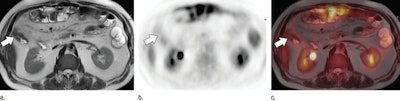
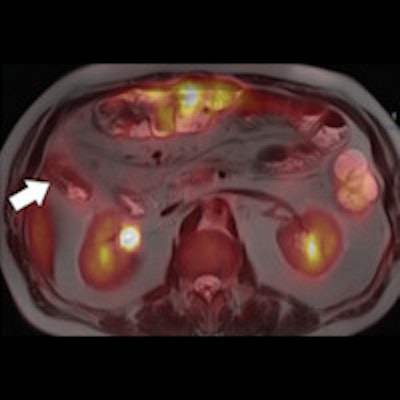
A 54-year-old man with Crohn's disease. Axial T2-weighted half-Fourier rapid acquisition with relaxation enhancement (RARE) MRI (a), axial PET image (b), and axial fused T2-weighted half-Fourier RARE PET/MRI (c) indicate a stricture (arrow) within the ascending colon. Images courtesy of Radiology.
The study also found signal intensity on T2-weighted images and ADC alone were inconclusive in telling the difference between patients with fibrosis and inflammation.
"On the basis of these initial results, PET/MR enterography may be a useful noninvasive imaging tool in patients with Crohn disease who have obstructive symptoms and a high clinical suspicion of strictures," Catalano and colleagues wrote.
The authors cited several limitations of the study, including the small number of patients and bowel segments in the research, noting that a larger study "would be advisable to confirm these preliminary results."
However, "PET/MR enterography offers a potential noninvasive technique for the differentiation of purely fibrotic strictures from mixed or inflammatory strictures," they concluded.