A radiomics model that incorporates T2-weighted MR enterography (MRE) exam data appears to improve the accuracy of pediatric Crohn's disease diagnosis, according to a study published August 2 in the American Journal of Roentgenology.
The group found ileal wall radiomic features to be strong predictors of Crohn's disease and that the radiomic model bested expert radiologist interpretation, noted corresponding author Jonathan Dillman, MD, of Cincinnati Children's Hospital in Ohio.
"A radiomic machine learning model predicted Crohn's disease diagnosis with better performance than two of three expert radiologists," he wrote.
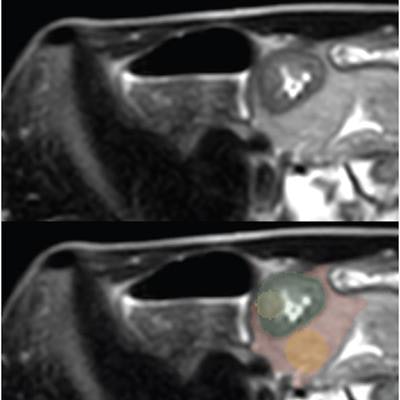
The study included data from 135 patients suspected of ileal Crohn's disease who underwent MR enterography (MRE) between December 2018 and October 2021; of these, 70 were eventually diagnosed with the condition. One radiologist chose two slices from each axial T2-weighted single-shot fast-spin echo (SSFSE) image that showed the greatest ileal wall thickening, then segmented four regions of interest and extracted radiomic features from these.
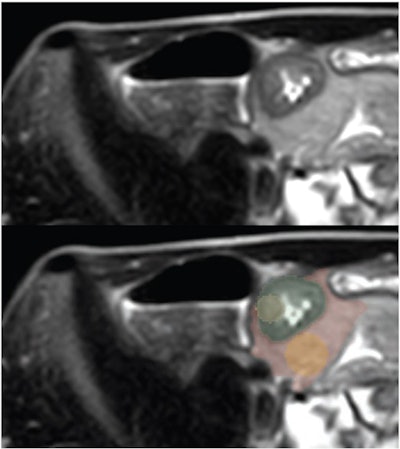 17-year-old patient with Crohn disease. Axial T2-weighted SSFSE images show greatest terminal thickness -- without (top) and with (bottom) four ROI segmentations. (Green = whole-bowel ROI; yellow = bowel-core ROI; red = whole-fat ROI; orange = fat-core ROI.) Image and caption courtesy of the American Journal of Roentgenology.
17-year-old patient with Crohn disease. Axial T2-weighted SSFSE images show greatest terminal thickness -- without (top) and with (bottom) four ROI segmentations. (Green = whole-bowel ROI; yellow = bowel-core ROI; red = whole-fat ROI; orange = fat-core ROI.) Image and caption courtesy of the American Journal of Roentgenology.Three pediatric abdominal radiologists flagged the presence of ileal Crohn's disease on these SSFSE images. The study's reference standard was the clinical diagnosis of ileal Crohn's disease following positive endoscopy and biopsy, the group explained.
The radiomic model that used a round bowel-wall region-of-interest in the greatest area of ileum thickening showed an AUC of 0.95 and accuracy of 89.6%. The best results were achieved, however, by a combination of the radiomic model with a model utilizing clinical factors such as age, sex, erythrocyte sedimentation rate, and C-reactive protein.
| Performance of three different models for identifying Crohn's disease | |||
| Measure | Clinical-only model | Radiomic-only model (using a bowel-wall region of interest) | Combination of bowel-core radiomic and clinical models |
| AUC | 0.85 | 0.95 | 0.98 |
| Accuracy | 80% | 89.6% | 93.5% |
The study also found that, with the help of a radiomic model, the three pediatric radiologists had accuracy rates for diagnosing Crohn's disease of 83.7%, 86.7%, and 88.1%.
The findings are promising, but further research is necessary, according to the authors.
"Clinical deployment of [the combined] model has the potential to decrease inter-radiologist variability and increase diagnostic accuracy for Crohn's disease," they concluded. "While the results are promising, future investigations are needed, including multi-center training and external validation, development of automated region-of-interest placement, and application of similar pipelines to other key clinical questions in Crohn's disease management, including prediction of treatment response, future complications, and need for surgery."
The complete study can be found here.