An AI model trained on Dixon MRI may help with large studies researching abdominal fat distribution in children, suggest Dutch findings published August 16 in the American Journal of Roentgenology.
Researchers led by Tong Wu, MD, from Erasmus University Medical Center in Rotterdam found that their model could successfully perform segmentation for subcutaneous adipose tissue (SAT) and visceral adipose tissue (VAT) when assessing fat distribution on MRI, along with ties between such distribution and clinical outcomes.
"The fat segmentations obtained by the model showed strong agreement with manual segmentations, as well as associations with anthropomorphic and [dual-energy x-ray absorptiometry]-derived measures," Wu and co-authors wrote.
Childhood obesity has become more commonplace around the world, with the consequences translating to health issues in adulthood. Previous research suggests that higher amounts of VAT are tied to a higher risk of cardiovascular disease, metabolic disease, and cancer. The researchers wrote that this means accurate, noninvasive methods are needed to quantify body fat distribution in children for better clinical outcomes.
Dixon MRI techniques have been investigated for their ability to analyze fat tissue. Here, coregistered water and fat images are obtained from differences in resonance frequencies of protons in water and fat.
For their study, Wu and colleagues wanted to develop and test an automated deep-learning method for SAT and VAT segmentation using Dixon MR images acquired from adolescents.
They trained, validated, and tested the model, a competitive dense fully convolutional network (2D-CDFNet), on data from participants in the Generation R Study. This prospective population-based cohort study in Rotterdam included 2,989 children with an average age of 13.5 years. The participants underwent investigational whole-body Dixon MRI after reaching age 13 years, during the study's follow-up phase. The model was trained to segment abdominal SAT and VAT using Dixon-based MRI.
Wu et al used Dice similarity coefficients and volumetric similarity to assess segmentation performance. From there, two observers independently performed subjective visual assessments of automated segmentations in 504 children. Also, the team computed Spearman coefficients in 2,820 children with complete data. These were computed between MRI measurements with body mass index (BMI) and dual-energy x-ray absorptiometry (DEXA)-based measures.
The researchers found that for the test dataset, the Dice similarity coefficient and volumetric similarity were 0.94 and 0.98 for SAT, respectively. For VAT, these measures were 0.85 and 0.92, respectively. These results indicate that the model demonstrated strong quantitative performance.
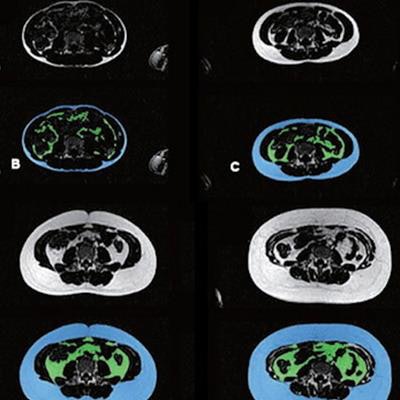
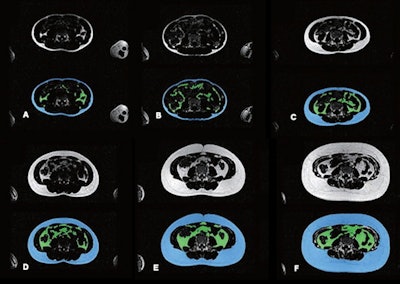 Example results show automated abdominal adipose tissue segmentation into SAT and VAT using Dixon MRI acquisitions in different children. In each image, top and bottom images represent fat-only images without (top) and with (bottom) segmentation. Blue areas denote SAT, and green area denotes VAT. Images A-F represent six children with varying body sizes and varying amounts of abdominal SAT and VAT. Images courtesy of ARRS.
Example results show automated abdominal adipose tissue segmentation into SAT and VAT using Dixon MRI acquisitions in different children. In each image, top and bottom images represent fat-only images without (top) and with (bottom) segmentation. Blue areas denote SAT, and green area denotes VAT. Images A-F represent six children with varying body sizes and varying amounts of abdominal SAT and VAT. Images courtesy of ARRS.The team also reported that the two observers assigned a score of 3, the best possible visual score, for SAT in 94% and 93% for undersegmentation proportion, and 99% and 99% for oversegmentation proportion. The observers also assigned a score of 3 for VAT in 99% and 99% for undersegmentation proportion and 95% and 97% for oversegmentation proportion. These findings indicate a strong qualitative performance by the model.
Finally, the researchers found that the correlations with SAT and VAT were 0.808 and 0.698 for BMI, and 0.941 and 0.801 for DEXA-derived fat mass.
Based on these results, the model could help with future large-scale research studying abdominal fat distribution on MRI, according to the authors. This could also mean investigating associations between abdominal fat distribution and other body composition measures or clinical outcomes.
The study can be found in its entirety here.