With its ability to achieve a high level of specificity, the combination of carbon-11-labeled Pittsburgh Compound B (PiB) with PET imaging is showing early promise in distinguishing meningiomas from other intracranial tumors, according to a study presented recently at RSNA 2016.
Researchers from the Mayo Clinic in Rochester, MN, are optimistic that PiB-PET could become a sensitive marker for intracranial meningioma and foster appropriate patient triage and treatment, without the need for invasive testing and the associated potential morbidity.
"The benefit with PiB so far seems to be its specificity," said lead author and neurologist Dr. Derek Johnson. "Meningiomas demonstrate activity on PiB-PET with high-level uptake that is specific for a variety of meningiomas."
Meningioma prevalence
Meningiomas are typically benign tumors that cause harm by pressing on the brain. They are the most common type of intracranial tumor and are present in approximately 1% of imaging studies and in as many as 3% of adult autopsies, Johnson told RSNA attendees.
 Dr. Derek Johnson of the Mayo Clinic
Dr. Derek Johnson of the Mayo ClinicMRI has been the primary option for diagnosing meningiomas, but the modality's lack of specificity can limit its efficacy among patients with a history of cancer.
"The problem is our current [imaging] tools lack specificity to make important and time-sensitive treatment decisions," Johnson said.
Meanwhile, PiB-PET is best known for its contribution to research on Alzheimer's disease, investigating the source of the condition. The compound adheres to beta-amyloid plaque deposits in the brain, which have been linked to dementia and cognitive impairment. Other research has suggested PiB-PET may be useful in identifying meningiomas and that some meningioma subtypes contain amyloid, but there is no consensus on this issue.
"The previous pathology in literature has been mixed on the topic, but overall it does not seem like there is or ought to be amyloid with meningioma," Johnson said. "It leads to the question: What is [PiB] binding to? Our aims were was to evaluate the test characteristics of PiB-PET in meningioma identification and assess the presence of beta-amyloid in meningiomas."
PiB revelations
The researchers retrospectively studied patients who underwent PiB-PET/CT at the Mayo Clinic between March 2006 and September 2015. They reviewed 2,472 patient records to identify those with intracranial tumors at least 5 mm in thickness and seen on contrast-enhanced MRI scans. Tumors also had to be confirmed by available pathology or by imaging characteristics as interpreted by board-certified neuroradiologists.
Of the 2,472 patients, 45 (1.8%) met the criteria for having a probable or confirmed intracranial tumor. There were 29 cases of meningioma (64%), as well as seven patients with vestibular schwannoma, four with pituitary macroadenoma, two with metastatic disease, two with an intraventricular mass, and one epidermoid tumor.
PiB uptake was significantly greater among the 29 patients with meningiomas, who had a mean maximum standardized uptake value (SUVmax) of 2.05 (standard deviation, 1.37). The second highest mean SUVmax was 1.40 (standard deviation, 0.72) for metastatic disease, followed by 1.37 (standard deviation, 0.54) for intraventricular masses.
Meningiomas also greatly differed in a lesion-to-cerebellum PiB uptake comparison. The mean SUVmax ratio for meningiomas was 2.12 (standard deviation, 0.70), compared with the second-highest result of 1.39 (standard deviation, 0.24) for intraventricular masses.
Lesion-to-cerebellum ratios above an optimum SUVmax ratio of 1.65 with an area under the curve (AUC) value of 0.91 accurately indicated meningioma. Results below the cutoff ratio indicated nonmeningiomas. For results at or above this ratio, sensitivity was 76%, specificity was 100%, positive predictive value was 100%, and negative predictive value was 70%.
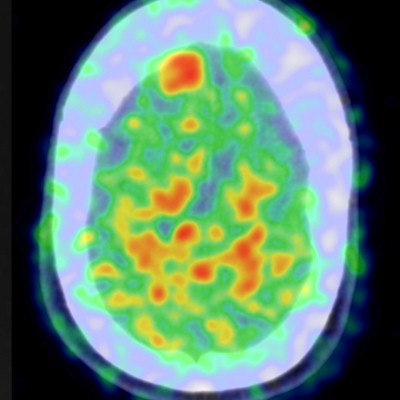
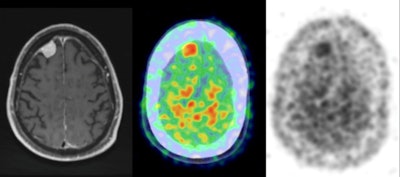 Postcontrast axial T1-weighted MRI demonstrates a right frontal meningioma (left), while the PET/CT axial color map fusion image (center) shows intense PiB activity within the meningioma. Also, an axial PET image (right) demonstrates intense PiB activity within the meningioma. Images courtesy of Dr. Derek Johnson.
Postcontrast axial T1-weighted MRI demonstrates a right frontal meningioma (left), while the PET/CT axial color map fusion image (center) shows intense PiB activity within the meningioma. Also, an axial PET image (right) demonstrates intense PiB activity within the meningioma. Images courtesy of Dr. Derek Johnson.Amyloid connection
So why does PiB localize to meningiomas? To explore that question, Johnson and colleagues took tissue samples from patients with meningiomas, vestibular schwannomas, and metastases and stained the specimens with a beta-amyloid antibody, which is widely used in clinical neuropathology practice; PiB, which is weakly fluorescent; and a highly fluorescent PiB analog.
The researchers discovered that PiB and the PiB analog both stained all seven meningiomas (100%) and none of the vestibular schwannoma and metastases samples. The beta-amyloid antibody produced no staining in the meningiomas or other samples.
"The pattern of staining with PiB and the highly fluorescent PiB analog is nuclear and perinuclear, whereas in a person with Alzheimer's disease [PiB] is binding to amyloid plaques, which are extracellular," Johnson explained. "So it does not answer the question 'What is [PiB] binding to?' but it certainly suggests what PiB is not binding to."
As for the next round of research, Johnson said there is the need for a prospective evaluation of additional meningioma "mimics" and other grades of meningioma as well.
"Our data is concordant with the literature that it is probably not amyloid that [PiB] is binding to, but something else that needs to be determined," he said. "We also should investigate [U.S. Food and Drug Administration]-approved amyloid radiotracers to see if they demonstrate a similar pattern."