SPECT/CT can be a valuable resource for diagnosing gastrointestinal and genitourinary bleeding in the emergency room setting, and it does so in a reasonable amount of additional time, according to a study from Stony Brook University.
Researchers found that SPECT/CT correctly identified the cause of bleeding in 22 (96%) of 23 patients who had inconclusive results from standard dynamic imaging studies. The hybrid modality was also precise in locating abnormalities and led to more accurate interventions for patients.
 Dr. Elham Safaie from Stony Brook University.
Dr. Elham Safaie from Stony Brook University."SPECT/CT has superior spatial resolution and accurate localization with the use of the CT component," said lead author Dr. Elham Safaie, a clinical assistant professor of radiology at Stony Brook School of Medicine. "This would lead to a definite diagnosis in complex cases and will lead to better patient management as a result."
Conventional imaging
Traditional nuclear medicine gastrointestinal and genitourinary studies to detect bleeding use dynamic and static or planar images to come to a diagnosis. However, these types of imaging modalities are often not sufficient to arrive at a final conclusion. By comparison, SPECT/CT is better at localizing the source of problem, while CT provides better definition of anatomy and higher spatial resolution.
"SPECT/CT, however, is sometimes time-consuming and is not used in most settings for emergency room cases," Safaie said during her presentation of the study at RSNA 2016.
In the retrospective study, the researchers reviewed 23 consecutive abdominal patients who were seen between July 2013 and March 2016 and whose initial studies in the emergency room were inconclusive. The patients underwent initial dynamic imaging, followed by SPECT/CT.
The exams performed included red blood cell (RBC) bleeding, hepatobiliary, Meckel's diverticulum, and renal studies.
SPECT/CT discoveries
SPECT/CT was performed at the end of dynamic imaging and deemed helpful in 22 (96%) of the 23 cases, allowing clinicians to identify the regional anatomy as the source of gastrointestinal bleeding in all six cases.
Of those six patients, four diagnoses of bleeding were in the large bowel and two were in the small bowel. One patient (17%) had both a small bowel and a peritoneal bleed, which was confirmed by surgery. Three patients (50%) had multiple prior studies performed, which were inconclusive before SPECT/CT.
SPECT/CT successfully localized nine (64%) biliary leaks among the 14 hepatobiliary studies. In addition, the modality confirmed three cases (21%) of atresia and excluded cholecystitis in two patients (14%) by identifying the gallbladder as the source of the bleeding.
Among the other patients, SPECT/CT was able to identify the precise location of a urinary leak in a renal transplant patient, but it was inconclusive for the lone Meckel's diverticulum study.
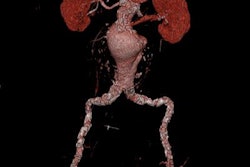
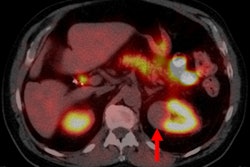
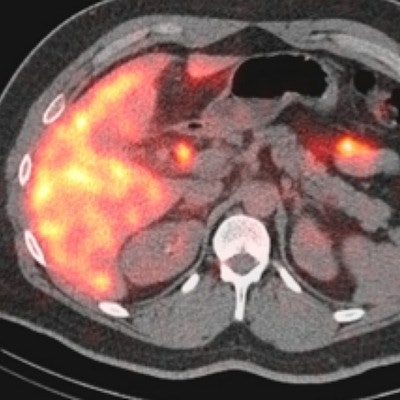
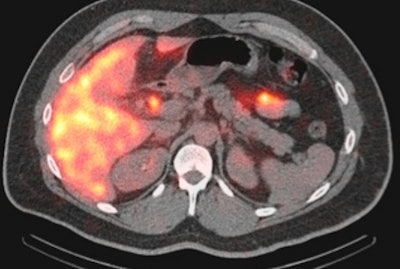 SPECT/CT image of a 35-year-old woman with a small bile leak at the cholecystectomy site. Image courtesy of Dr. Elham Safaie.
SPECT/CT image of a 35-year-old woman with a small bile leak at the cholecystectomy site. Image courtesy of Dr. Elham Safaie.The average additional scan time for SPECT/CT ranged from 20 to 30 minutes, depending on the patient's dose and his or her situation, Safaie said. That added scan time is "reasonable even in an emergency setting," she added.
"Our findings demonstrated that adding SPECT/CT to standard gastrointestinal and urinary dynamic imaging supplements conventional imaging in equivocal patients for anatomic localization and subsequent intervention," Safaie concluded in the presentation. "SPECT/CT is effective because it makes use of CT that is not usually used for many general nuclear medicine studies. It also allows for anatomical correlation of the given pathologies."