Chinese and U.S. researchers have developed a novel PET tracer that may enhance the management of patients with non-small cell lung cancer (NSCLC), according to a study published online in the March 7 issue of Science Translational Medicine.
The researchers from Harbin Medical University in China and Stanford University in Palo Alto, CA, have synthesized a PET tracer that can yield noninvasive estimates of a tumor's epidermal growth factor receptor (EGFR) mutation status -- a critical factor in stratifying patients who would benefit from treatment with EGFR tyrosine kinase inhibitors (TKIs).
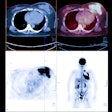
The F-18 MPG tracer, which includes compounds of fluorophenyl, fluoroethoxy, and methoxyquinazolin, was found in human testing to be 84.3% accurate for identifying NSCLC patients with EGFR-activating mutant tumors (Sci Transl Med, March 7, 2018, Vol. 10:431).
"We wanted to develop a novel strategy with PET imaging for noninvasively determining EGFR mutation status in real-time, predict NSCLC patients who may benefit from EGFR-TKI therapy, and monitor EGFR-TKI treatment outcome," said co-senior author Dr. Baozhong Shen, a professor of radiology at Harbin Medical University, in a statement.
Current techniques to assess EGFR mutation status require biopsy, but these methods have a high failure rate and poor reproducibility, according to the researchers. It can also be difficult to assess EGFR mutation status over space and time due to intra- and intertumor heterogeneity.
Plasma samples of NSCLC patients also have been used, but this method is inconsistent for determining EGFR mutation status and can't reveal whether the tumor is the primary tumor or a metastatic site.
After achieving high sensitivity and specificity in detecting activated EGFR mutational status in mouse models, the researchers then evaluated the technique on 75 human patients with NSCLC. The PET/CT scans with F-18 MPG yielded an accuracy of 84.3% for identifying EGFR-activating primary tumors or metastases.
In addition, the researchers observed good patient outcomes after EGFR-TKI therapy in a subgroup with very high pretreatment F-18 MPG uptake, suggesting that F-18 MPG PET/CT can predict treatment response.
"There currently are no methods to predict EGFR-TKI therapy response in patients and design effective EGFR-TKI therapies when a genetic test is not feasible or ambiguous." Shen said. "With [F-18 MPG] PET/CT imaging, we were able to quantitate EGFR-activating mutation status in NSCLC patients (primary tumor or metastatic) and directly determine/visualize the location(s) and morphology of the NSCLCs."