Can you name the best strategies to optimize FDG-PET/CT to assess lung disease? If not, researchers from imaging centers in the U.S. and the U.K. have provided their consensus recommendations on how best to proceed in a study published online September 18 in the Journal of Nuclear Medicine.
Their advice covers patient preparation, the use dynamic or static PET, image analyses, thoughts on image reconstruction, and overcoming common obstacles, such as respiratory motion effects.
"To help harmonize the acquisition and analysis and promote reproducibility, acquisition protocol and analysis method details were collated from seven PET centers," wrote the authors, led by Dr. Delphine Chen from the University of Washington and the Seattle Cancer Care Alliance. "Based on this information and discussions among the authors, the consensus recommendations reported here on patient preparation, choice of dynamic versus static imaging, image reconstruction, and image analysis reporting were reached."
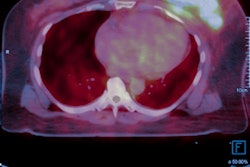
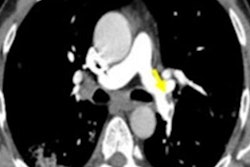
FDG-PET has been used extensively in both clinical and research settings to determine pulmonary function and monitor disease progression and treatment success in patients with lung disease, particularly afflictions that adversely affect the airways and/or vasculature. Currently, however, there are "no widely accepted standard acquisition protocols and imaging data analysis methods for pulmonary FDG-PET/CT in these diseases, resulting in disparate approaches," the authors noted.
Hence, the researchers collected acquisition protocols and image analysis processes from their facilities to devise best practice recommendations for maximizing PET results for whole and regional lung imaging using static and/or dynamic PET.
For example, the investigators determined that patient preparation should include the following protocols:
- Patients should be given only plain water a minimum of six hours before scanning to maximize FDG glucose uptake.
- Establish a lower limit of 4 mmol/L to avoid requiring glucose to prevent hypoglycemia.
- The CT field-of-view should be clear of patients' arms -- preferably positioned over their heads -- to reduce inaccurate attenuation correction across the chest.
- Ensure patient comfort with amenities, such as a continuous oxygen supply and pillows or memory foam padding under their arms for support and enhanced blood circulation.
When calculating FDG dose for a particular study, the authors advised following the European Association of Nuclear Medicine's guidelines for clinical oncologic PET, while research studies should use the minimal tracer dose needed to achieve "sufficient image quality to meet the study objectives."
Additionally, PET lung imaging can be challenging due to movement of the lungs while breathing, which also results in varying air volume. Collectively, the authors most often utilized a "breath hold at gentle end-expiration or at mid-expiration for the CT scan" approach to minimize PET and CT misregistration. "Prescan coaching to familiarize the patient with breathing instructions [also] improved compliance and is thus recommended," they added.
As one would expect, choosing static and dynamic PET depends on the goal. A static PET image offers details on scarring and inflammation and can be performed approximately 60 minutes after tracer administration. Dynamic PET provides additional information on low-level inflammation, as well as the lung's components, with image acquisition beginning immediately after injection and continuing for 45 to 90 minutes.
As for image reconstruction, Chen and colleagues noted there currently are available a number of different algorithms "leading to different noise and image characteristics," but they declined to make any recommendations, citing a lack of available data.
"To improve both reproducibility and potential for data pooling between centers and reproducibility for studies within a given center, investigators using PET/CT in studies of lung disease are urged to follow the recommendations presented in this manuscript when designing, conducting, and reporting studies," Chen and colleagues concluded. "As highlighted above, ample opportunities for investigation exist to improve the methods used to acquire and analyze lung PET/CT images."