By providing detail on perfusion in the brain, SPECT can predict how long patients with epilepsy will live free of seizures after brain surgery, according to a study published September 30 in the Journal of Nuclear Medicine.
German researchers analyzed SPECT scans of patients prior to having temporal lobe epilepsy surgery to remove the area causing their seizures. They found patients with a "favorable ictal perfusion pattern" on SPECT can live seizure-free for years, compared with months in patients who didn't show the pattern prior to surgery.
"The expression of this pattern is easily computed for new ictal SPECT images and, therefore, might be used to support the decision for or against temporal lobe surgery in clinical patient care," wrote a team led by first author Dr. Jila Taherpour of University Medical Center Hamburg-Eppendorf.
Drugs to prevent seizures stop working in about a third of people with temporal lobe epilepsy. In patients who subsequently undergo surgery, seizures return in approximately 40%. In addition, psychiatric disorders, visual field defects, and cognitive impairment occur in about 20% of patients after surgery.
SPECT of ictal perfusion is performed on epileptic patients during seizures to localize the area of the brain to be removed prior to surgery. Radiopharmaceutical uptake can reveal abnormal blood flow, or specific perfusion patterns, during the scan.
Previous research on the predictive value of the technique has been qualitative, relying on the visual classification of ictal perfusion patterns, and this can vary among interpreting physicians, according to the authors. In this prospective study, Taherpour and colleagues aimed to determine if ictal perfusion SPECT could provide unbiased, quantitative evidence to predict how effective the surgery may be.
The researchers identified 18 patients who responded to temporal lobe epilepsy surgery after 12 months and 18 patients whose seizures had returned to some degree. They analyzed 16 ictal perfusion SPECT covariance patterns among patients who underwent scans (Symbia T2 or e.cam, Siemens Healthineers) prior to surgery.
The team found one out of the 16 covariance patterns was expressed differently between responders and nonresponders. This "favorable ictal perfusion pattern" resembled the typical ictal perfusion pattern in mesial temporal lobe epilepsy and provided an area under the receiver operating characteristic curve of 0.744 for predicting seizure freedom 12 months after surgery, the authors wrote.
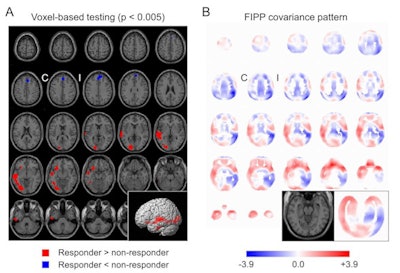 Statistical maps of hyperperfusion (red) and hypoperfusion (blue) obtained by conventional univariate voxel-based one-sided t-tests corrected for injection latency, thresholded at p = 0.005 and overlaid on the statistical parametric mapping single subject template (A). Part B shows the "favorable ictal perfusion pattern." (I/C = ipsilateral/contralateral to temporal lobe epilepsy surgery). Image courtesy of the Journal of Nuclear Medicine.
Statistical maps of hyperperfusion (red) and hypoperfusion (blue) obtained by conventional univariate voxel-based one-sided t-tests corrected for injection latency, thresholded at p = 0.005 and overlaid on the statistical parametric mapping single subject template (A). Part B shows the "favorable ictal perfusion pattern." (I/C = ipsilateral/contralateral to temporal lobe epilepsy surgery). Image courtesy of the Journal of Nuclear Medicine.A Kaplan-Meier analysis revealed a statistical trend toward longer freedom from seizures in patients who expressed the favorable pattern. The median estimated seizure-free time was 48 months in patients with positive expression score versus six months in patients with a negative expression score, the researchers found.
"The expression of the 'favorable ictal perfusion pattern' identified by covariance analysis of ictal brain perfusion SPECT provides independent information for the prediction of seizure freedom after temporal lobe epilepsy surgery," they wrote.
Classification of ictal perfusion patterns for predicting surgery outcome is not common in clinical routine, the authors noted. Yet importantly, the computation of the perfusion pattern in this study is fully automatic and does not require special expertise, in contrast to visual interpretation of ictal SPECT images, the team stated.
"This simplifies widespread clinical use," the group concluded.