F-18 fluoroestradiol (FES) PET/CT imaging could improve patient management in women with invasive lobular carcinoma (ILC) breast cancer, according to a presentation Sunday morning at the RSNA 2021 meeting.
A team led by radiologist Dr. Matthew Covington of the University of Utah's Huntsman Cancer Institute found FES-PET/CT detected all tumor sites of biopsy-proven ILC in a small group of newly diagnosed women. The finding offers hope for patients for whom conventional imaging is frequently inaccurate.
"[FES-PET/CT] showed very good ability to discriminate between metastatic and nonmetastatic axillary lymph nodes, and both FES and FDG detected additional disease in the breast at a high rate," Covington said.
ILC is the second most common type of breast cancer after invasive ductal carcinoma. More than 180,000 women in the U.S. find out they have invasive breast cancer each year, according to the American Cancer Society. ILC is often difficult to detect on physical examination and standard imaging, such as mammography, ultrasound, CT, and FDG-PET/CT, according to the researchers.
Moreover, data on ILC are sparse because nearly all invasive breast cancer studies have grouped ductal and lobular carcinoma together, Covington added.
"I think that's a problem because lobular is unique. It is its own cancer," he said.
In this ongoing pilot study, Covington and colleagues studied results from nine women with biopsy-proven ILC from any body site. Patients were also offered FDG-PET/CT scans within four weeks of enrollment. Positive uptake at sites of biopsy-proven ILC on FES-PET/CT was defined as SUVmax > 1.5.
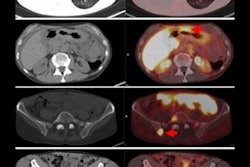
Biopsies established 14 sites of ILC. Of the 14 sites, 13 were estrogen receptor (ER)-positive and one was triple negative. All 14 demonstrated positive uptake on FES-PET/CT (average SUVmax of 4.7, with a range from 1.5 to 12.7). FDG-PET/CT was performed in six patients with 10 lesions. On FDG-PET/CT, nine of 10 lesions (90%) demonstrated positive uptake, the team found.
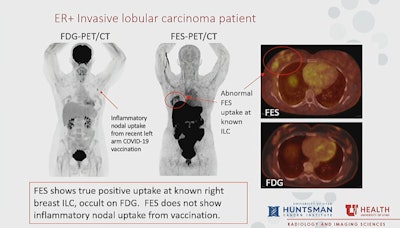 Image courtesy of Dr. Matthew Covington.
Image courtesy of Dr. Matthew Covington.In addition, axillary nodal metastatic disease was confirmed on pathology in seven patients and FES-PET/CT showed 100% sensitivity and 100% specificity detecting these lesions, compared with a sensitivity of 67% and specificity of 100% for FDG-PET/CT, the researchers found.
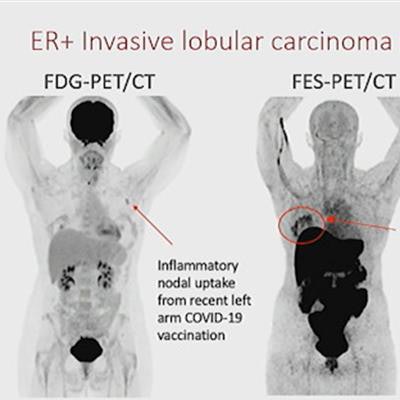
Covington also noted studies that show FDG uptake in lymph nodes in patients undergoing PET/CT scans after COVID-19 vaccinations -- a problem that may confound the interpretation of imaging. One patient in this study had inflammatory lymph node uptake on FDG-PET/CT from a recent vaccination that did not show on FES-PET/CT.
"An advantage of FES especially in this era of COVID-19 is that we don't see inflammatory nodal uptake," Covington said.
Patients with ILC could benefit from this new approach, according to Covington, given that compared with invasive ductal carcinoma, ILC is more frequently occult or undersized on imaging, is detected at later stages, and results in more frequent repeat surgeries for positive margins.
"I think FES-PET/CT may change patient management for initial staging of ER-positive ILC patients," Covington concluded.
The study is ongoing, Covington noted, adding that larger multicenter studies are needed to clarify the role of FES-PET/CT for the evaluation and management of ER-positive breast malignancy.
To that end, plans have been launched to initiate a much larger study, he said.