As if a midlife crisis weren’t bad enough: The breakdown of myelin in the brain that comes with aging could contribute to the onset of Alzheimer's disease, a leading brain researcher reports in the Neurobiology of Aging.
"Our analysis of brain tissue and MRI (scans) indicates that white-matter brain myelin begins to break down in the 30s and 40s, the brain’s time of peak performance, and sets up the situation for the development of Alzheimer’s," said Dr. George Bartzokis, director of the Memory Disorders and Alzheimer's Disease Clinic and clinical core director of the Alzheimer's Disease Research Center, both at the University of California, Los Angeles.
Bartzokis noted that the human body was designed to myelinate through its lifespan. However, since medical advances have extended the lifespan, the brain's capacity to operate in an efficient manner has not kept pace.
"Our challenge is to determine how extend the peak performance phase so the mind will function as long as the body," he said.
For this study, Bartzokis analyzed both MR images and post-mortem tissue data. He found that genetic factors, as well as increasing cholesterol and iron levels in middle age, contribute to the degradation of myelin.
Complex neurological connections, which enable humans to process thoughts at the highest levels, deteriorate as myelin degenerates. As a result, myelin breakdown should be addressed in middle age, he said. By the time Alzheimer's disease becomes evident at ages 60-80, it could be impossible to alter the course of disease.
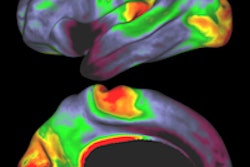
"The under-appreciation of the importance of human myelination is perhaps best demonstrated by the paucity of postmortem or in vivo maps of myelination and the dearth of detail," Bartzokis explained. "The advent of in vivo neuroimaging methods that can assess myelination on a regional basis is beginning to correct this gap in our knowledge and possibly provide impetus for quantitative post-mortem and imaging approaches to gather region and network/neurotransmitter-specific information." (Neurobiology of Aging, January 2004, Vol. 25:1, pp. 5-18).
"These methods will allow neuroscientists to supersede the existing sketchy maps of myelination and produce the age-specific three-dimensional maps of normal myelination that are needed for a better understanding of the disease processes," he added. Bartzokis noted that potential preventive therapies for Alzheimer’s could include activities to keep the mind active and stimulating the production of myelin.
In one of six accompanying commentaries, Dr. James Connor, professor of neuroscience and anatomy at Pennsylvania State University College of Medicine in Hershey wrote: "The types of neurological events in which white matter involvement is seen are detailed in the Bartzokis article. However, frequently the white matter involvement is considered secondary or of less neurological consequence than accompanying gray matter damage."
"Perhaps, in view of the strong supporting data discussed in the Bartzokis article, the white matter involvement will be given greater consideration," Connor said. "As argued, continual degradation of white matter and fragmentation of myelin could result in continued or exacerbation of an inflammatory reaction that could prove resistant to therapeutic interventions that do not specifically target this region."
By Bruce SylvesterAuntMinnie.com contributing writer
January 8, 2004
Related Reading
Functional brain abnormalities present early in epsilon-4 carriers, December 16, 2003
Trial questions PET's cost-effectiveness for Alzheimer's diagnosis, September 16, 2003
Scans suggest why education prevents Alzheimer’s, August 8, 2003
Alzheimer’s brains show features of immaturity, May 8, 2003
Imaging’s role still evolving in dementia diagnosis, April 29, 2003
Copyright © 2004 AuntMinnie.com