Bone bruises are thought to result from microfractures of the medullar trabeculae. They are often radiographically occult and hidden on arthroscopy. In a new paper in the September issue of American Journal of Roentgenology, Dutch radiologists looked at whether the natural course of bone bruises, as seen on MRI, had any prognostic value.
The patient population consisted of 134 subjects (ages 18-65) who had sustained an acute trauma of the knee less than five weeks before consulting their general practitioner about knee pain. Patient workload and sports load were assessed. MRI was done on a 1.5-tesla scanner (Signa Horizon LX IT, GE Healthcare, Chalfont St. Giles, U.K.) and included the following sequences: sagittal T1-weighted fast spin echo (FSE), sagittal intermediate-weighted FSE, and coronal T2-weighted fat-suppressed imaging. The latter sequence was used to read the follow-up MR exams done in 80 patients after the first MRI.
"The rationale for performing follow-up scanning at approximately three weeks, 10 weeks, six months, and one year after the initial scanning was that this schedule was expected to enable an accurate survival analysis, taking into account both the fast-resolving lesions and the more slowly resolving lesions," wrote Dr. Simone Boks and colleagues from Erasmus Medical Center in Rotterdam, the Diaconessenhuis Meppel in Meppel, and the Medical Centre Rijnmond-Zuid in Rotterdam (AJR, September 2007, Vol. 189:3, pp. 556-562).
A bone bruise was identified as an area of abnormally high signal intensity in the subchondral bone or marrow on T2-weighted fat-suppressed imaging. Bone bruise severity was classified by the percentage of bone volume involved (ranging from less than 25% to more than 75%). On follow-up, a single bone bruise was considered resolved, while the collective resolution of multiple bone bruises (in a single patient) was treated as healed.
 |
 |
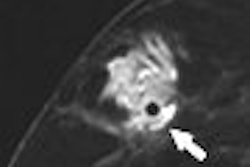
| A 31-year-old man with fast resolution of bone bruise, reticular lesion type. Coronal T2-weighted fast-suppressed images (TR/TE, 12/3,700; fat saturation; section thickness, 3 mm; field-of-view, 180 x 135 mm; matrix, 385 x 224) show fast resolution of bone bruise from baseline (above), to three-week follow-up (middle), and at nine-week follow-up (below). |
 |
| Boks SS, Vroegindeweij D, Koes BW, Bernsen RMD, Hunink MGM, Bierma-Zeinstra SMA, "MRI Follow-Up of Posttraumatic Bone Bruises in General Practice" (AJR; 189: 10.2214/AJR.07.2276). |
The median healing time was 42.1 weeks, according to the results, and was unaffected by workload and sports. Follow-up was completed in 72 of 134 patients, with 22 continuing to demonstrate a bone bruise after one year.
In patients with osteoarthritis, the healing time was twice as long as those without osteoarthritis, the authors stated, with the disease acting as a "clear prognostic variable" for the presence of bone bruise at six months and one year. Finally, while the number of bone bruises prolonged the healing time, the severity of the bone bruise did not affect the injury's natural course, they explained.
"Our results show that bone bruise healing is mainly related to the presence of osteoarthritis," the authors concluded. In addition, "the higher the number of (bone bruises), the more likely that there will be one slowly resolving lesion."
The authors noted that the patients' general practitioners were not told of the MR results so imaging did not influence treatment planning. However, they stressed that "for daily practice, it is important to recognize that bone bruises take a relatively long time to dissipate.... Prognosis is mainly influenced by the presence of osteoarthritis.... Future studies must establish whether the presence of a bone bruise is related to clinical pain."
By Shalmali Pal
AuntMinnie.com staff writer
August 22, 2007
Related Reading
Glucosamine attenuates bone changes in experimental osteoarthritis, June 7, 2007
MR arthrography depicts tears, instability in triangular fibrocartilage complex, January 19, 2007
Copyright © 2007 AuntMinnie.com