On the whole, MR imaging negotiates the twists and turns of the knees with the greatest of ease. But there is one type of injury where MRI often hits a roadblock: meniscal tears. A recent study took a closer look at why these tears are sometimes missed at MRI, and whether certain clinical factors are in the modality's blind spot.
Dr. Arthur De Smet and Rajat Mukherjee from the University of Wisconsin School of Medicine and Public Health in Madison reviewed more than 1,000 medical records for patients who underwent knee MRI. De Smet is from the medical school's department of radiology, while Mukherjee is from the department of statistics.
Based on the selection criteria, the retrospective review included 483 patients. All imaging was done on a 1.5-tesla scanner (Signa, GE Healthcare, Chalfont St. Giles, U.K.). The protocol included coronal T1-weighted, coronal fat-saturated proton density-weighted, sagittal proton density-weighted, and sagittal T2-weighted fat-saturated imaging sequences.
The authors chose six clinical variables as factors that may have been associated with difficulty in diagnosing a tear:
- Patient age
- Relationship to trauma
- Delay between onset of symptoms and MR study
- Delay between MR and arthroscopy
- Exam sensitivity based on image quality
- Location and type of lateral meniscal tear and anterior cruciate ligament (ACL) tear
Records were reviewed to determine the original MRI interpretation and findings at knee arthroscopy. "Our arthroscopic surgeons classify meniscal tears as being flap, complex, horizontal, longitudinal peripheral, radial, root, and bucket handle in pattern and localize a tear as being in the anterior horn, body, posterior horn, or a combination of these three locations or in the meniscal root," they explained (American Journal of Roentgenology, January 2008, Vol. 190: 1, pp. 22-26).
According to the results, 36 of 189 patients had lateral meniscal tears at arthroscopy that were missed in the MR exam. The authors found no significant difference in patient age, the delay between onset of symptoms and MR study, or the delay between MR and arthroscopy. However, when the time between symptom onset and MR exam was more than 90 days, 24% of lateral meniscal tears were missed.
Overall, MR's sensitivity for diagnosing lateral meniscal tears was 81%, while specificity was 88%. The authors noted that the sensitivity did vary with tear location. For instance, if the tear involved more than one-third of the meniscus, sensitivity was 100%. The sensitivity of MR for finding a tear in the body of the meniscus root was 82% and 83% in the root of the meniscus root. The sensitivity was 73% for detecting tears in the posterior horn. This difference in sensitivity was most likely because tears involving at least one-third of the meniscus are larger, De Smet and Mukherjee stated.
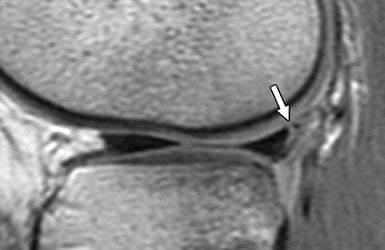 |
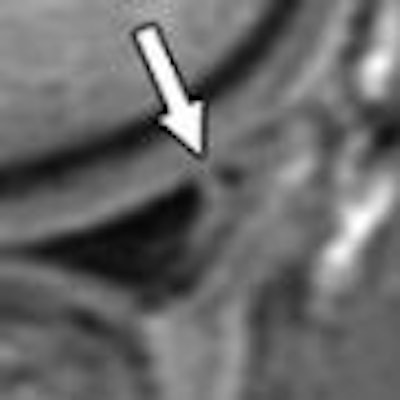
| A 15-year-old girl with originally missed longitudinal peripheral tear of posterior horn of lateral meniscus seen on retrospective review. Tear was repaired with sutures. Sagittal fast spin-echo proton density-weighted image shows peripheral longitudinal tear with vertical orientation (arrow). De Smet AA, Mukherjee R, "Clinical, MRI, and Arthroscopic Findings Associated With Failure to Diagnose a Lateral Meniscal Tear on Knee MRI" (AJR 2007; 190:22-26). |
In other findings, for 305 medial meniscal tears, MR turned in a sensitivity of 97% and a specificity of 86%. In 84 patients with ACL tears and lateral meniscal tears, MR's sensitivity was 76%. For the 105 patients without ACL tears, sensitivity was 85%.
Finally, 23 of the 36 missed tears could not be seen retrospectively even with knowledge of the type, location, and extent of the tear. Four of these were flap tears, four were peripheral longitudinal tears, and six were root tears. In some cases, the tear type was not specified, the authors noted.
"One unexpected finding was that eight (89%) of the nine tears not classified as a specific tear type in the arthroscopy report were missed," they wrote. "It is difficult to hypothesize why these tears were missed on MRI," adding that it may have just been a clerical oversight, but that "it is puzzling why sensitivity was significantly lower in these cases."
While the authors could not come to any specific conclusions about why tears were missed, they cautioned that many had a longitudinal peripheral pattern with a vertical tear orientation. These tears are particularly unstable and can progress to bucket handle detachment, they cautioned.
In their conclusion, they cited a 2006 study by Drs. Thomas Magee and David Williams that reported better results with 3-tesla fast spin-echo MRI for diagnosing meniscal tears (AJR, October 2006, Vol. 187:4., pp. 881-886).
"If this accuracy is confirmed in additional studies ... a 3-(tesla) magnet may prove to be the best way to use MRI to diagnose lateral meniscal tears," De Smet and Mukherjee stated.
A newer study from the Rheinische Friedrich-Wilhelms-Universität in Bonn, Germany, found that 3-tesla MR was particularly useful for assessing horizontal and complex tears of the medial meniscus, and that the higher field strength magnet also showed higher accuracy for the lateral meniscus (Archives of Orthopaedic and Trauma Surgery, October 30, 2007).
In an e-mail interview, De Smet answered some additional questions on this study from AuntMinnie.com.
AuntMinnie: In a previous paper, your group described the "two-slice-touch" rule to increase the positive-predictive value (PPV) for diagnosing meniscal tears. The rule "classifies a meniscus as torn if there are two or more MR images with abnormal findings and as possibly torn if there is only one MR image with an abnormal finding." Was the two-slice-touch rule followed when the MR studies used in the current AJR paper were read originally? (AJR, October 2006, Vol. 187:4, pp. 911-914).
De Smet: Yes. However, for this report, tears not identified at MRI were being evaluated so we considered all definite and possible tears as MR indications of a meniscal tear.
How important are the MRI findings clinically in terms of guiding treatment for meniscal tears? Are the majority of patients headed to surgery regardless of what is or isn't seen on the MRI?
This is actually a question for an orthopedic surgeon. As a generalization, the decision to perform a surgery is based on a combination of the patient's history, findings on physical examination by the surgeon, and the MR results.
Normally, if there is a negative MRI, surgery would not be performed unless the surgeon feels, based on the history and physical examination, there is a still a reasonable likelihood that there is a meniscal tear.
However, it is important to recognize that the patient may have another indication for surgery such an ACL tear, which would have resulted in performing surgery. Thus, while a lateral meniscal tear was not detected at MRI, an ACL tear was diagnosed so the patient had surgery at which the missed lateral tear was detected.
Are you currently working with 3-tesla MR for diagnosing lateral meniscal tears?
Yes. I've begun a study comparing 3-tesla and 1.5-tesla, which should be submitted for publication in four to six months.
By Shalmali Pal
AuntMinnie.com staff writer
February 8, 2007
Related Reading
Studies uphold MRI's role in meniscal tears, propose new sequences, May 16, 2007
From tears to TKA: The ins and outs of knee MRI, September 5, 2006
Copyright © 2008 AuntMinnie.com



.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=100&q=70&w=100)



.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=167&q=70&w=250)











