A commercially available software program that automatically quantifies the extent of brain atrophy on MRI scans can help physicians better determine the risk of developing Alzheimer's disease in patients with mild cognitive impairment (MCI), according to a study published online October 12 in Neurology.
Researchers from the University of California, San Diego (UCSD) and the University of Gothenburg in Sweden used the software in conjunction with two clinically available measures for predicting the onset of dementia: degree of learning impairment and abnormal biomarker levels of cerebrospinal fluid (CSF).
They found that 85% of patients with both greater learning impairment and atrophy as measured by the MRI software developed dementia within three years, compared with only 5% of patients who were negative for both conditions. The study was led by Dr. David Heister, PhD, from UCSD's department of radiology.
Volumetric MRI
Previous studies have determined that the severity of cognitive impairment, as well as abnormal CSF biomarker levels and atrophy as detected by MRI measurements of brain volume (volumetric MRI, or vMRI), can predict conversion to Alzheimer's disease and patient outcome, according to the authors. But while CSF and vMRI can be used to rule out causes of dementia, such as cerebral infections and inflammatory disorders, the two techniques are not typically included in routine clinical workups of patients with mild cognitive impairment, in part due to the difficultly in generating vMRI measurements.
"Methodologic barriers have prevented implementation of vMRI in clinical practice," Heister and colleagues wrote. "However, large-scale studies, such as the Alzheimer's Disease Neuroimaging Initiative (ADNI) and clinical trials incorporating vMRI as outcome measures, have assisted in overcoming these barriers."
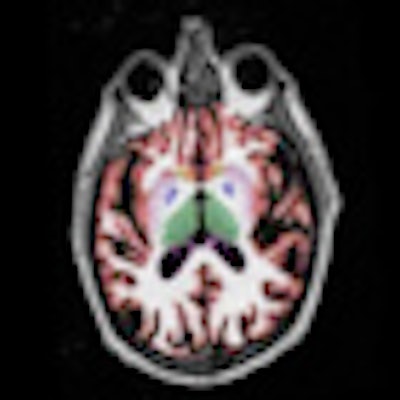
A commercially available software application (NeuroQuant, CorTechs Labs) is capable of generating automated measurements of brain volume that can be used in conjunction with clinical findings. The software performs automatic labeling, visualization, and volumetric quantification of segmentable brain structures.
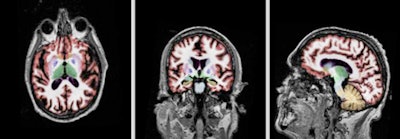 |
| Sagittal, axial, and coronal plane views (left to right) of a volumetric MRI scan using NeuroQuant on a patient with Alzheimer's. Images courtesy of CorTechs Labs and Dr. James Brewer, PhD, UCSD. |
The researchers used the database from the ADNI to collect information from August 2005 to October 2010 on 215 healthy control subjects and 192 people with mild Alzheimer's disease. The healthy control group excluded 11 individuals who developed mild cognitive impairment or Alzheimer's disease during the course of the study.
The researchers then categorized the 192 subjects with MCI into positive and negative risk groups to predict the onset of dementia based on three criteria: the degree of learning impairment, the degree of atrophy in the medial temporal lobe of the brain as measured on volumetric MRI, and the levels of CSF biomarkers that are associated with Alzheimer's disease.
Risk factors
Patients with mild cognitive impairment who tested positive for each risk factor showed "significantly greater hazard of converting to Alzheimer's disease than those testing negative," the authors wrote.
In addition, combining information from any two risk factors dramatically improved risk discrimination, with the combination of learning impairment and medial temporal atrophy on vMRI providing the best ability to predict outcome.
Senior study author Linda McEvoy, PhD, from UCSD's radiology department, noted that when risk factors were analyzed separately, patients who were positive for any one risk factor showed greater chances of developing dementia than patients who tested negative for that same factor.
Subjects who tested negative for severe learning impairment and for atrophy at vMRI were at very low risk of converting to Alzheimer's disease, with 95% of these patients remaining stable through the three-year follow-up period.
By comparison, individuals with both atrophy and learning impairment were at very high risk to develop Alzheimer's disease, with only 15% of these patients having no signs of dementia after three years. Almost 50% of the patients were discordant for these two measures and had an elevated risk of developing Alzheimer's, a level that was not as great as when both factors were positive. Approximately 50% of these patients had no signs of dementia after three years.
Survival time
Median survival time was significantly shorter for patients at risk due to atrophy on vMRI, whether they had that risk factor alone (survival time of 15.5 months) or in combination with other factors (15 months), compared to patients at risk from other measures or a combination of measures (range, 20.5 to 28.5 months), the authors wrote.
UCSD has been using the protocol clinically for more than three years, and it has changed the way patients are assessed and managed for MCI and Alzheimer's disease.
Study co-author Dr. James Brewer, PhD, a neurologist and faculty member at UCSD, noted that while heart damage can be detected with physical markers, there is no similar measure for brain deterioration. Volumetric MRI can look directly at the brain to determine if critical structures are deteriorating, he added.
The authors cited several limitations of the study, including the fact that the mildly cognitive impaired subjects in the study were not representative of the general clinical population.
"There is a strong need to gain more experience with currently available clinical tools for aiding in the prediction of Alzheimer's disease in the clinical setting, so that if disease-modifying treatments become available, these techniques will have been validated on typical clinical populations and be ready for routine use," Heister and colleagues wrote.



.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=100&q=70&w=100)



.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=167&q=70&w=250)