Wednesday, November 28 | 11:00 a.m.-11:10 a.m. | SSK10-04 | Room E451A
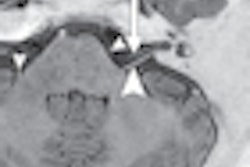
Preoperative MRI using metal artifact suppression parameters can visualize extra-articular fluid collection, and is a reliable modality to show soft-tissue necrosis in patients presenting for additional surgery following primary total hip arthroplasty with metal-on-metal components.Those conclusions come from researchers at Massachusetts General Hospital (MGH), who added that T1-weighted MRI may also be valuable in characterizing fluid collections.
"Evolving data suggest that failure of metal-on-metal hip replacements, in contrast to more commonly used metal-on-polyethylene designs, is related to soft-tissue injury," said lead study author Dr. Carson Campe, a resident in MGH's department of radiology. "Currently, the best imaging modality for evaluating soft tissues is MRI. These two factors, combined with the limitations of other modalities, make MRI the most effective imaging tool for evaluating patients with metal-on-metal implants."
This study analyzed 13 hips in 12 patients (average age, 59 years) who had both MRI and revision surgery performed at MGH between April 2011 and March 2012. The time between metal-on-metal arthroplasty and MRI averaged 27 months. In all 12 patients, the MR protocol included metal artifact suppression parameters.
All patients were symptomatic due to pain and/or mechanical symptoms and failed conservative treatment.
Operative findings included extra-articular collections in 10 (77%) cases and periarticular soft-tissue necrosis in all 13 cases. MRI showed 10 (100%) extra-articular collections. In nine of 10 collections, T1-weighted MRI signal intensity was increased compared with signal intensity of fluid in the bladder.
"The data we present in this abstract are an initial attempt to identify imaging findings that may indicate metal-on-metal prosthesis failure or correlate with a risk of future failure," Campe said. "Through presentation of our data, we hope to encourage the use of MRI in evaluation of metal-on-metal patients and stimulate investigations that may reveal MRI findings specific for reaction to metal and implant failure."
Campe and colleagues are continuing their research on the use of MRI for metal-on-metal components.
"We hope to identify imaging findings that correlate with intraoperative findings and clinical failure, as well as modify MRI techniques to optimize imaging yield and reduce metal artifact," he added. "Imaging shows great promise in evaluating these patients but requires further validation as a diagnostic tool."