MRI measurements of the amount of plaque in the abdominal aorta and the thickness of its wall are associated with future cardiovascular events, such as a heart attack or stroke, according to a study published online June 18 in Radiology.
Researchers from the University of Texas Southwestern Medical Center found that among 2,122 participants, 825 (39%) had aortic plaque and 143 (6.7%) experienced a cardiovascular event during a mean follow-up period of 7.8 years.
The findings show that atherosclerosis in an artery outside of the heart can be an independent predictor of adverse cardiovascular events, said lead author Dr. Christopher Maroules, a radiology resident at the medical center, in a statement.
"MRI is a promising tool for quantifying atherosclerosis through plaque and arterial wall thickness measurements," he added.
Coronary and cerebrovascular atherosclerotic disease has been linked to adverse cardiovascular outcomes; however, less is known about asymptomatic aortic atherosclerosis, the authors noted (Radiology, June 18, 2013).
Dallas Heart Study
Maroules and colleagues culled the Dallas Heart Study for their cohort. The Dallas Heart Study included people ages 18 to 65 years who participated in a detailed survey about their medical and family history.
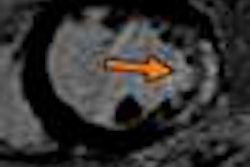
In the current study, 2,122 participants successfully underwent abdominal aortic 1.5-tesla MRI scans on a whole-body system (Intera, Philips Healthcare). Aortic atherosclerosis was measured by calculating the mean abdominal aortic wall thickness and the amount of plaque buildup, which was referred to as the aortic plaque burden.
The study population included 1,188 women (56%) and 934 men, who had a mean age of 44 years (± 10 years). Follow-up included monitoring for cardiovascular deaths, nonfatal cardiac events, and nonfatal extracardiac vascular events (i.e., events in noncardiac arteries such as in the brain or abdomen) over a mean period of 7.8 years (± 1.5 years).
Plaque presence
MRI discovered aortic plaque in 825 subjects (39%) in the study, and 361 individuals (17%) had both prevalent aortic plaque and high mean aortic wall thickness. In addition, 446 subjects (21%) had aortic plaque alone, 170 (8%) had high mean aortic wall thickness alone, and 1,167 (55%) had neither condition.
One hundred forty-three subjects (6.7%) experienced a cardiovascular event during the mean period of 7.8 years. Of those individuals, 34 (1.6%) had a fatal cardiovascular event, 73 (3.4%) experienced a nonfatal cardiac event, and 46 (2.2%) had a nonfatal extracardiac vascular event.
Other findings included the following:
- Hypercholesterolemia was positively associated with aortic plaque.
- Body mass index of more than 30 kg/m2 was negatively associated with aortic plaque.
- Low HDL cholesterol level was positively associated with mean aortic wall thickness but not with aortic plaque burden.
- Mean aortic wall thickness was associated with increased risk for composite cardiovascular events and nonfatal extracardiac vascular events.
In addition, age, male sex, smoking, and hypertension were positively associated with both measures of aortic atherosclerosis.
"Our results suggest that mean aortic wall thickness but not aortic plaque burden is a significant independent predictor of composite cardiovascular events, and both mean aortic wall thickness and aortic plaque burden are significant independent predictors of extracardiac events," Maroules and colleagues wrote.
"These results validate the prognostic implications of these subclinical aortic atherosclerosis measures and clarify the relevance of these measures for specific clinical manifestations of cardiovascular disease," they added.
The authors cautioned that the relatively small number of cardiovascular events in the study limited their ability to explore associations in patient subgroups. "Future studies with longer surveillance periods will be necessary to evaluate age, sex, and ethnic-specific differences in the prognostic value of these measurements," they wrote.