Using MRI, British researchers have debunked a common misconception that a rare disorder that adversely affects the reproductive system of younger women prevents development of the uterus, according to a study published online August 13 in Radiology.
MR images confirmed that women with the condition, known as Mayer-Rokitansky-Kuster-Hauser (MRKH) syndrome, may have large uteri with no conventional structure (defined as rudimentary uteri in this study) that can mimic normal postpubertal uteri. By discovering MRKH syndrome in young women, MRI can prompt the diagnosis of the disorder at an earlier age, avoid an invasive procedure, and lead to appropriate counseling.
"It is a common misconception that women with MRKH syndrome have no uterus, even though the presence of rudimentary uterine structures or buds is well described in [previous] literature," wrote lead author Dr. Margaret Anne Hall-Craggs and colleagues. "Our study showed rudimentary uteri in nearly 93% of patients, which was very similar to laparoscopic findings [in previous research]" (Radiology, August 13, 2013).
Interrupted development
MRKH syndrome is a malformation of the female genital tract due to interrupted embryonic development of the paramesonephric ducts, leading to underdevelopment or incomplete development of the uterus and the upper two-thirds of the vagina. Girls sometimes discover they have the condition when they fail to begin menstruating after reaching puberty.
As the authors wrote, MRKH syndrome has "devastating implications for fertility and sexual intercourse in young women. It is essential that the diagnosis be reached quickly and accurately to allow clinical and psychologic input."
Physicians at University College London Hospital primarily use pelvic ultrasound to investigate and diagnose MRKH syndrome, but MRI is utilized when ultrasound findings are inconclusive or when there are clinical conditions, such as pelvic pain.
During this retrospective study from 2001 to 2011, the researchers identified 215 patients with MRKH syndrome. Of that total, 66 (31%) received MRI scans of the pelvis. The age of the patients who underwent MRI (either at University College London Hospital or referring hospitals) ranged from 14 to 40 years, with a mean age of 21.1 years.
All MRI scans were performed on a 1.5-tesla scanner (Symphony or Avanto, Siemens Healthcare, at University College London Hospital) with T2-weighted imaging in three planes and transverse T1-weighted imaging. Forty-four patients received intravenous contrast, while 22 did not receive contrast.
Hall-Craggs reviewed the MRI results for the presence, site, volumes, and differentiation into layers (myometrium, junctional zone, and endometrium) of uterine remnants. Ovarian volumes and positions were assessed and vaginal length was measured.
MRI findings
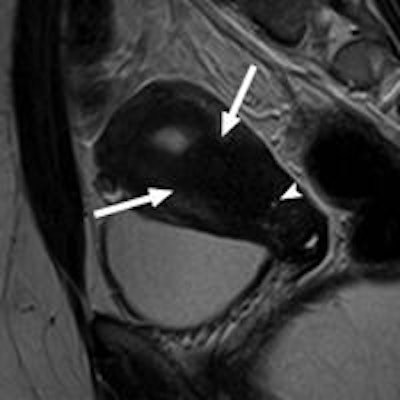
A total of 115 rudimentary uteri were found in the 66 patients, with one or two rudimentary uteri in 61 women (92%). Of those 61 subjects, 54 (82%) had bilateral rudimentary uteri and seven (11%) had unilateral rudimentary uteri. Five individuals (8%) had no uterine remnants.
Mean uterine volume was 6.4 mL (range, 0.4 mL to 80.2 mL), with 18 uteri having a volume greater than 10 mL.
MRI also detected two uteri containing intraluminal blood, and two uteri showed signs of adenomyosis, indicating functioning endometrial tissue. The same two patients with an indication of adenomyosis were experiencing pain.
In addition, 22 patients had no discernible vagina (dimple or less). Of the 44 patients with a vagina, the mean length was 2.0 cm (range, 1.0 cm to 6.5 cm).
"Two important findings in our study are the large size (larger than 80 mL) and variable appearances of some of the rudimentary uteri," Hall-Craggs and colleagues noted. "Although large, these uteri did not have a conventional structure; there was no cervix, and the uterine shape was not organized into a fundus and body with ostia. Although some differentiation into layers was seen, this generally occupied a small central proportion of the uterus."
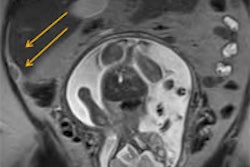
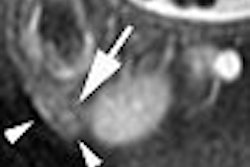
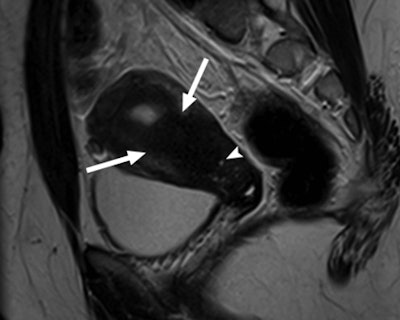 Sagittal T2-weighted MRI of a 24-year-old woman with cyclical pelvic pain in the largest rudimentary uterus (80 mL). Image shows three-layer differentiation and extensive adenomyosis with thickening of the junctional zone (arrows) and small hemorrhagic foci (arrowhead). Image courtesy of Radiology.
Sagittal T2-weighted MRI of a 24-year-old woman with cyclical pelvic pain in the largest rudimentary uterus (80 mL). Image shows three-layer differentiation and extensive adenomyosis with thickening of the junctional zone (arrows) and small hemorrhagic foci (arrowhead). Image courtesy of Radiology.The study also found that one or both ovaries were not in their correct location (ectopic) in 27 patients. "Consequently, 41% of patients had one or more ectopic ovary, and this finding is more common than previously described," the authors wrote.
Correct identification and location of the ovaries is critical, especially in women with MRKH syndrome, who can still achieve fertility through in vitro fertilization and use of a surrogate, they added.
The authors cited several limitations to the study. Because not every patient underwent an MRI scan, there was a selection bias against the most typical cases, and the researchers were more apt to refer patients with pain or large uteri for imaging. There also was only one reader (Hall-Craggs), so there was no corroboration of measurements and description of uteri.