After three decades of dedication to the care and treatment of children in Malawi who have cerebral malaria, a group of researchers from around the globe for the first time confirmed that brain swelling is the primary reason why some patients die within days from the condition.
The landmark study, published in the March 19 issue of the New England Journal of Medicine, suggests that this increased brain volume adds pressure at the base of the skull and prevents children from breathing. The finding offers significant insight into why approximately one-third of children with cerebral malaria die and the other two-thirds survive (NEJM, Vol. 372:12, pp. 1126-1137).
Senior author Dr. Terrie Taylor has been studying the pathogenesis of cerebral malaria in Malawian children since 1986. She and Dr. Malcolm Molyneux, a study co-author from the Liverpool School of Tropical Medicine, established the Blantyre Malaria Project at Queen Elizabeth Central Hospital.
 Dr. Terrie Taylor of Michigan State University and Queen Elizabeth Central Hospital.
Dr. Terrie Taylor of Michigan State University and Queen Elizabeth Central Hospital.Taylor spends half her year at the College of Osteopathic Medicine at Michigan State University and the other half in Queen Elizabeth's department of pediatrics and child health. The modern, government-owned, 1,000-bed hospital offers various pediatric services as well as adult care.
"It all began with a request for help by the Ministry of Health in Malawi to highlight the situation of malaria in children," Taylor told AuntMinnie.com. "It was fortunate for us that they chose something so fascinating."
In the summer of 2008, GE Healthcare donated a 0.35-tesla MRI scanner (Signa Ovation 0.35T, which is no longer commercially available) to the facility. The system was ready for the malaria season of 2009, which is when Taylor and colleagues began using it to investigate brain swelling and other potential causes of fatal cerebral malaria.
Types of malaria
There are basically two kinds of malaria, Taylor explained. "Uncomplicated" malaria is characterized by fever, headaches, nausea, vomiting, muscle aches, and pains, similar to the flu. "Grown-up Malawians describe that as total body pain," she said. "Having had that once, I agree."
A few patients develop "complicated" malaria, which is more severe and includes anemia and cerebral malaria. Taylor estimated that approximately one-third of the in-hospital deaths at Queen Elizabeth are due to malaria.
The disease is contracted through the bite of the female Anopheles mosquito, which delivers a parasite into the bloodstream of the person bitten. The parasite then travels to the liver and eventually the red blood cells. (Taylor calls it the "Voldemort of parasites," a reference to Lord Voldemort, the arch-villain in the "Harry Potter" series.)
While in the red blood cells, the parasite begins its reproductive cycle, a process that takes 48 hours from initial infection of the red blood cells to rupture of a cell, releasing 32 new parasites, Taylor said. The parasite can be detected through a simple blood sample.
Normally, the parasites would be eradicated when the blood flows through the spleen, but in the second half of the 48-hour life cycle, the parasitized red cells develop the ability to stick to the inside of blood vessels (the endothelial lining) and avoid the spleen.
"So the upshot of that is when you do these finger-prick samples of blood, you only see the young parasites," Taylor said. "You don't see the old ones because they are tucked away."
What makes the condition even more nefarious, she added, is that people infected with malaria can show no signs or symptoms.
"That capacity to tolerate an infection without becoming symptomatic is acquired over many years of being exposed to malaria," she said. "And it is not necessarily true that any parasites you find are responsible for the symptoms of the patient."
Finding the cause
In the NEJM study, Taylor and colleagues assessed 348 children who were admitted to the hospital with cerebral malaria. Of those patients, 168 met the study criteria, including the presence of retinopathy. Twenty-five children (15%) died, and of this group, 21 (84%) had evidence of severe brain swelling on MRI when they were admitted to the hospital.
"Looking at all the clinical features of the kids, one of our observations was that the retinopathy finding in the back of the eye matched up perfectly with the autopsy findings," Taylor said. "The kids who had changes in the back of their eyes had sequestration in their brain, and the kids who had normal eye exams had no sequestration in the brain and another cause of death. Those [retinopathy-positive] kids had true cerebral malaria."
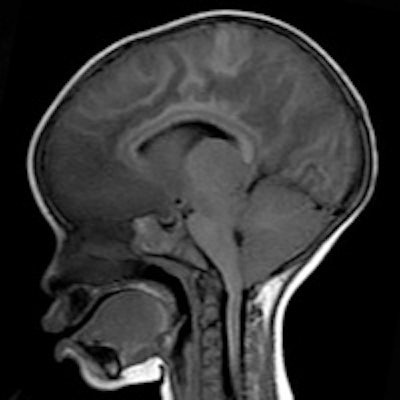
MR images revealed brain swelling in 39 (27%) of the 143 survivors, but that swelling eventually decreased after two to three days among the survivors. Taylor described that result as a "triumphant moment" in the study.
 MRI shows normal brain volume in a 14-month-old girl at one-month follow-up. Images courtesy of Michigan State University and GE Healthcare.
MRI shows normal brain volume in a 14-month-old girl at one-month follow-up. Images courtesy of Michigan State University and GE Healthcare.More importantly, the first piece of critical evidence came from one of the first patients scanned on the newly donated MRI. The child came to the hospital with typical cerebral malaria symptoms, including retinopathy. The comatose patient had an MRI on day 1 and a second one on day 2, but died four hours after the second scan.
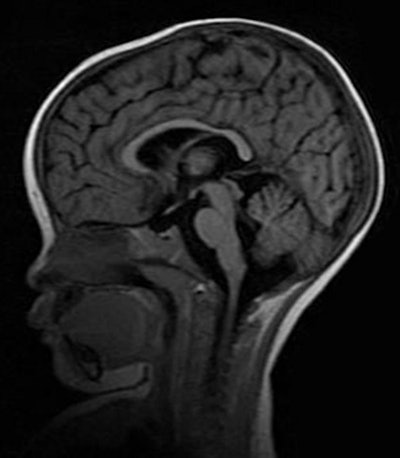
While the MRI scan at autopsy revealed a swollen brain, there was no evidence of severe expansion. However, the MRI acquired during the first 24 hours after admittance showed clear evidence of the brain pushing down through a narrow hole, known as the foramen magnum, at the base of the skull.
"That area gets mushed and compressed if the brain is pushed out, and causes breathing to stop," Taylor said. "We would always look for that, but we never saw it. We could see it on the MRI and we instantly knew what happened. We never, ever would have seen it had we not captured it during life with the MRI."
 MR image shows increased brain volume in a 19-month-old girl with retinopathy-positive cerebral malaria.
MR image shows increased brain volume in a 19-month-old girl with retinopathy-positive cerebral malaria.Because of the pressure on the foramen magnum, the retinopathy-positive patients with cerebral malaria inevitably died because they stopped breathing.
"Their heartbeat goes on; we can actually breathe for them by putting a mask over their mouth and nose and using a bag to push in air, but they do not start breathing again," she said.
The biggest tragedy is that the hospital has no ventilators, and the patients die within an hour of when they stop breathing, she added.
Future focus
Now that researchers have this additional knowledge about cerebral malaria, the plan is to follow two parallel tracks.
"One is the academic track, which is to elucidate the causes of the brain swelling. It is not immediately obvious why," Taylor said. "There are four potential possibilities, and we would like to work through each of them."
Approximately two-thirds of the children whose brains swell recover and return to normal with only traditional antimalaria treatment.
"We give them antimalaria drugs, blood transfusion, anticonvulsants, treat the fever, etc., but we don't do any special treatment with the brain," Taylor said. "Even without anything special, the brain volume goes back to normal among the survivors. Two-thirds of those with brain swelling do survive, while the other one-third does not."
The second objective is the clinical track, to help the children when they stop breathing. For these patients, Taylor speculated that breathing assistance, as with ventilators, might tide them over during their vulnerable period.
However, another major challenge is not knowing how far the cerebral malaria has progressed when these patients are admitted to the hospital.
"They show up at the hospital at all different stages of malaria," Taylor said. "We really don't have any way of knowing how long a given child has been infected."
Also contributing to the NEJM paper were researchers from the Malawi-Liverpool-Wellcome Trust Clinical Research Programme, University of Malawi College of Medicine, Harvard University School of Public Health, Brigham and Women's Hospital, and University of California, San Diego.




















