Using a novel motion-tracking MRI technique, researchers from Johns Hopkins University have uncovered new evidence that reduced function in the left atrium of the heart may be a sign of increased stroke risk in patients with or without atrial fibrillation.
The findings, published online April 27 in the Journal of the American Heart Association, would seem to contradict current clinical thinking that the abnormal beating of the upper chambers of the heart during atrial fibrillation can cause the formation of blood clots that lead to stroke.
The Johns Hopkins researchers said the current rationale doesn't explain why many people with atrial fibrillation never have strokes, or why individuals with a history of atrial fibrillation have no evidence of abnormal rhythms within a month or so of having a stroke. In other words, patients with altered function in the left atrium may be at risk for stroke, whether or not they have atrial fibrillation.
 Dr. Hiroshi Ashikaga, PhD, from Johns Hopkins University.
Dr. Hiroshi Ashikaga, PhD, from Johns Hopkins University.While these results are preliminary, lead author and heart rhythm specialist Dr. Hiroshi Ashikaga, PhD, and colleagues believe that motion-tracking MRI tests of the left atrium can improve the assessment of stroke risk and provide more effective therapy for these patients.
How it's done
The MRI technique uses a 1.5-tesla MRI scanner (Magnetom Avanto, Siemens Healthcare) with semiautomated multimodality tissue-tracking (MTT) software (Toshiba America Medical Systems) to analyze cardiac muscle movement. The software was developed with the help of study co-author Dr. Joao Lima, who has published previous research using the MRI technique to assess left atrium function (Radiology, December 2014, Vol. 273:3, pp. 703-713).
"The good thing about this imaging technique is that it is noninvasive," Ashikaga, an assistant professor of medicine and biomedical engineering at Johns Hopkins, told AuntMinnie.com. "Traditionally, for people who have atrial fibrillation, we estimate the risk of a stroke and decide whether or not to start [them on] a blood thinner to prevent a stroke. Sometimes, there has to be a diagnosis of atrial fibrillation to start the [treatment] process, but this kind of approach does not help people who present with a stroke as the first manifestation of atrial fibrillation."
Oftentimes, patients who have a stroke feel no signs of atrial fibrillation or irregular heartbeat, and they require prolonged electrocardiogram monitoring to determine if there is any abnormality, he added.
"So if we can look at the left atrial function in anyone, it is very easy because we don't have to wait for atrial fibrillation to occur," Ashikaga said. "If we can screen people who are at higher risk of a stroke, we can discuss therapy based on the result."
Ashikaga's study analyzed 169 patients with a history of atrial fibrillation at the time of preablation cardiac MRI. The patients had an average age of 59 years (range, 49-69 years), 74% of them were male, and 29% had persistent atrial fibrillation.
Of the subjects, 18 had a prior history of stroke or transient ischemic attack (TIA) at the time of their cardiac MRI scan. The remaining 151 patents had no history of stroke or TIA and were in the control group.
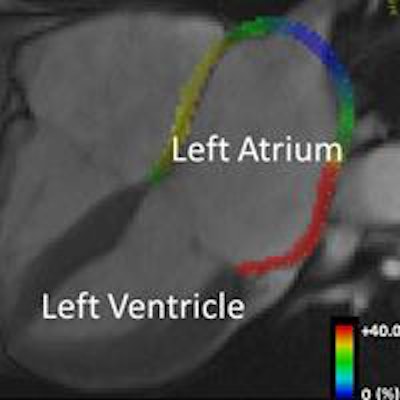
In their review of motion and MR images, the researchers found that the left atrium of patients with a history of stroke or TIA was noticeably less able to empty blood from the atrium into the left ventricle. This so-called "conduit" function contributed an average of 35% of ventricular filling per minute in patients with a history of stroke or TIA, compared with 46% per minute among the control subjects.
In addition, the left atria were larger in patients with a history of stroke or TIA, with an average volume of 52 mL/m2, compared with 44 mL/m2 in the control group. Also, the left atria of patients with a history of stroke or TIA had worse overall ability to contract with each heartbeat (booster pump function), meaning that the heart muscle was less elastic and less able to account for strain.
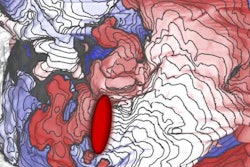
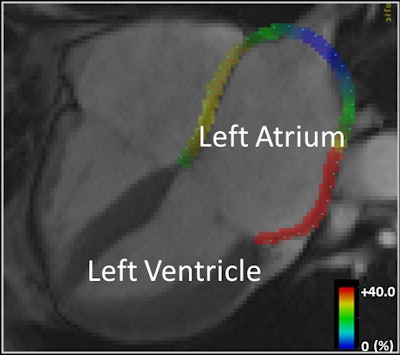 Motion-tracking MRI shows the heart wall of the left atrium highlighted in color (representing 0% to 40%) based on how much it has stretched from baseline. Image courtesy of Dr. Hiroshi Ashikaga, PhD.
Motion-tracking MRI shows the heart wall of the left atrium highlighted in color (representing 0% to 40%) based on how much it has stretched from baseline. Image courtesy of Dr. Hiroshi Ashikaga, PhD."Our findings are particularly important because, to our knowledge, this is the first report to demonstrate the significant contribution of the left atrium reservoir function to stroke in atrial fibrillation patients during sinus rhythm [or the normal beating of the heart]," the authors wrote.
So which patients might benefit most from this MR imaging technique?
"That is the $64,000 question," Ashikaga said. "This is a very promising result, but it has not been tested prospectively. We want to do it for all patients, but there are a few questions. For example, which patients would benefit from having this kind of test? And what kind of outcome can we expect? We don't yet know those things."
Ashikaga and colleagues are already planning several prospective studies to examine left atrial function in people with atrial fibrillation, those at high risk of atrial fibrillation, and those who do not have atrial fibrillation.