3D heart models based on MRI scans allowed for the virtual simulation of existing and future irregular heartbeats in patients with atrial fibrillation in a new study, published online August 19 in Nature Biomedical Engineering. The models helped pinpoint distinct regions in the patients' heart that would benefit most from ablation therapy.
One of the most common causes of irregular heartbeats is atrial fibrillation, which is typically treated via catheter ablation. This minimally invasive procedure entails applying radiofrequency energy to cardiac tissue in a trial-and-error process of eliminating erratic signals.
The traditional "one-size-fits-all" ablation approach does not take into account the high variability in heart rhythm disorders and often fails to deliver reasonable outcomes in patients with persistent forms of atrial fibrillation, prompting repeat treatment, researchers from Johns Hopkins University noted.
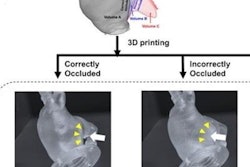
Seeking to personalize ablation therapy, the group developed a new technique, optimal target identification via modeling of arrhythmogenesis (OPTIMA), for determining preoperatively the precise location of erratic heart signals. The technique involves creating individually tailored 3D models of the heart atria from patients' late gadolinium-enhanced MRI scans and then using computational modeling to simulate all possible arrhythmias that could arise on these models.
"The beauty of working with such [3D heart] replicas is that we could test for and predict where irregular heartbeats persist in ways we never could in the clinic," said study co-author Natalia Trayanova, PhD, director of the university's computational cardiology laboratory, in a statement.
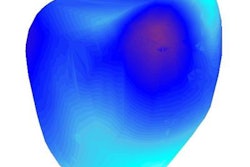
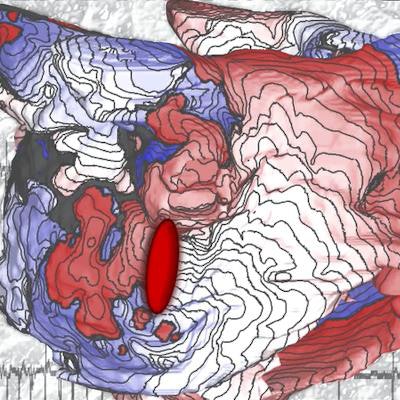
In a small-scale prospective trial, Trayanova and colleagues used their technique to simulate arrhythmias dozens of times on the 3D heart atria models of 10 patients with persistent atrial fibrillation. The simulations enabled them to generate a map of each heart that indicated all the regions requiring radiofrequency treatment. Clinicians then used this information to guide catheter ablation for the patients. The entire process of simulation and treatment for each patient took roughly one week, though the researchers believe they will be able to shorten this period to a single day in the near future.
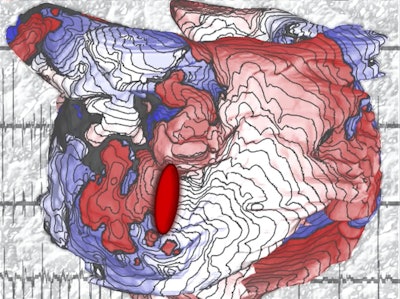 Depiction of a map from a 3D model of the heart atrium. Image courtesy of Patrick Boyle, PhD, and Natalia Trayanova, PhD, of Johns Hopkins University.
Depiction of a map from a 3D model of the heart atrium. Image courtesy of Patrick Boyle, PhD, and Natalia Trayanova, PhD, of Johns Hopkins University.After more than 300 days of observation, they found no recurrence of atrial fibrillation in any of the patients. One of the patients did return for a follow-up ablation procedure but it was to resolve a much more simple arrhythmia.
"I'm very optimistic that this personalized simulation-driven approach will prove to be the missing link needed to markedly improve catheter ablation outcomes in patients with more advanced forms of atrial fibrillation," co-author Dr. Hugh Calkins said. "This new approach may transform [the] current approach to catheter ablation of atrial fibrillation."
The efficacy of the 3D model simulation in this preliminary study demonstrates its potential to improve the treatment of heart rhythm disorders considerably beyond the 50% success rate of the current standard of care, according to Trayanova. "[It] is an exciting example of how engineering technology can be used in the clinic to help make treatment more accurate and spare patients from multiple costly, and sometimes risky, procedures," she said.