Researchers from the University of Pittsburgh Medical Center (UPMC) have uncovered distinct injury patterns in the brain using diffusion-tensor MRI (DTI-MRI) in people with concussion-related depression or anxiety. Results of the new study were published online June 16 in Radiology.
The findings could provide insight into how abnormalities occur after trauma and how treatment for nontrauma patients with neuropsychological symptoms might benefit some concussion patients, according to the group.
The study was spurred by UPMC's symptom-based treatment approach for patients with mild traumatic brain injury. The clinicians believe that if they target a patient's specific symptoms and treat them accordingly, concussed patients will have much better outcomes.
"The overarching theme of our research is that patients with a concussion have to be treated individually based on their symptoms," lead author Dr. Lea Alhilali, an assistant professor of radiology, told AuntMinnie.com. "It is important to glean what the patient's symptoms are and treat those specific symptoms."
DTI and the brain
This area of research with DTI-MRI is not new to Alhilali and colleagues. In 2013, they found that sleep-wake disturbances in patients with mild traumatic brain injury correlated with abnormalities in the parahippocampal region of the brain (Radiology, October 2013, Vol. 269:1, pp. 249-257).
Also, a 2014 study with DTI-MRI identified parts of the brain that cause people with mild traumatic brain injury to become dizzy or develop vision problems.
"We have this question of concussed patients, which is whether or not different symptoms are related to different injuries. Are they different clinical manifestations of the same injury or related to severities of the injuries?" Alhilali said. "So we've been looking at a lot of postconcussion symptoms to see if there are specific injuries that we can recognize that are associated with a given symptom."
UPMC has a large sports concussion center, which often uses conventional MRI for its injured patients.
"Usually, conventional MRI does not show any abnormalities," she said. "It is very frustrating for us as radiologists, the clinicians treating the patients, and the patients themselves that MRI can't answer the question about what is causing their symptoms."
In the current study, participants came from UPMC's electronic medical record, which was used to identify DTI scans performed for mild traumatic brain injury between January 2006 and January 2014. Subjects were between 10 and 50 years of age; the researchers excluded those who had a history of a neuropsychiatric illness or substance abuse, an abnormal CT or conventional MRI, or missing DTI results or neurocognitive assessment information.
The final cohort consisted of 45 patients with mild traumatic brain injury who had neuropsychiatric symptoms. Of this group, 38 people exhibited irritability, 32 had depression, and 18 had anxiety; 10 patients met the criteria for all three conditions (Radiology, June 16, 2015).
The study also included 29 control subjects with mild traumatic brain injury but no signs of neuropsychiatric symptoms. Including other concussion patients as a control group greatly helped the study, Alhilali said, because a similar population with similar risk factors will produce more reliable results.
Conventional MRI and DTI scans were performed on a 1.5-tesla MRI system (Signa, GE Healthcare) with an eight-channel head coil.
DTI-MRI measures the movement of water molecules in tissue and white-matter brain regions through fractional anisotropy to determine disruptions in flow. The lower the fractional anisotropy value, the more likely there is a microstructural abnormality.
"All the nerves in the brain are connected through white matter," Alhilali explained. "Diffusion-tensor imaging can detect abnormalities in these connections between different brain regions that other MR imaging techniques cannot detect."
DTI revelations
In the comparison with control subjects, DTI showed decreased fractional anisotropy in the superior longitudinal fasciculus, white matter around the nucleus accumbens, and anterior limb of the internal capsule in patients with mild traumatic brain injury and depression.
"The regions that we found were abnormal in patients with depression after trauma are actually very similar to regions that are abnormal in patients with nontraumatic major depressive disorder," she said.
That finding prompted the researchers to question whether there is a common pathology behind traumatic and nontraumatic depression.
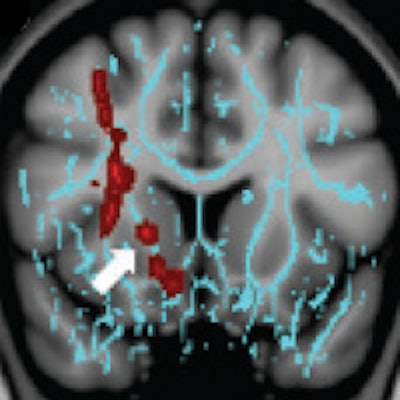
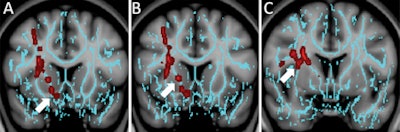 Diffusion-tensor images show how patients with depression have significantly decreased fractional anisotropy in the region of the right nucleus accumbens (A) (arrow) and the anterior limb of the internal capsule (B) (arrow) and superior longitudinal fasciculus (C) (arrow). The regions are involved in depressive disorders in nontraumatic and traumatic settings. Images courtesy of Radiology.
Diffusion-tensor images show how patients with depression have significantly decreased fractional anisotropy in the region of the right nucleus accumbens (A) (arrow) and the anterior limb of the internal capsule (B) (arrow) and superior longitudinal fasciculus (C) (arrow). The regions are involved in depressive disorders in nontraumatic and traumatic settings. Images courtesy of Radiology.The concussed patients with anxiety had diminished fractional anisotropy in the vermis, compared with the controls. Interestingly, while irritability is a common symptom after concussion, the researchers found no regions of significantly decreased fractional anisotropy in the concussed patients with irritability.
In explaining the lack of a difference, Alhilali surmised that while some postconcussion symptoms may be associated with a specific focal injury, perhaps not all of them are.
"There may be a component of organic brain injury, as well as the patient's ability to deal with the injury," that may have influenced this result, she said.
Another notable finding was that injury in the nucleus accumbens region was associated with recovery time in the concussed patients with depression. The nucleus accumbens essentially serves as the brain's reward center and is often abnormal in patients with a major depressive disorder.
"It was interesting to us that the more severe the injury was in the nucleus accumbens, the longer it took for [patients] to return to their baseline," Alhilali said. "It suggests that the nucleus accumbens plays a very important role in any sort of depressive symptom, and it might provide a target for future research in terms of treating both traumatic and nontraumatic depressive disorders."
Additional research
As for the clinical significance of the findings, the study shows that treatments already being used in the nontraumatic setting could potentially help concussed patients, Alhilali said. For example, pharmacologic treatment for nontraumatic depression may help patients who are depressed after a concussion.
"On the flip side, finding a very different injury in patients with anxiety disorder after trauma and those in the general population may indicate that medications used for nontraumatic anxiety patients may not be as effective in patients who have anxiety after concussion," she said.
The researchers plan to compare the traumatic and nontraumatic patient groups to further investigate abnormalities with depression and anxiety.




















