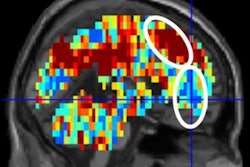
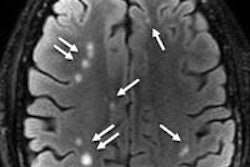
MRI scans have linked increased brain connectivity in people with traumatic brain injury (TBI) to depression and cognitive issues, according to a study published online November 4 in Frontiers in Neurology: Neurotrauma.
Researchers at the Center for BrainHealth at the University of Texas at Dallas found the heightened activity between multiple areas of the brain and the amygdala, a part of the brain responsible for emotional processing. These brain connectivity patterns also helped predict the type of depressive symptoms that study subjects experienced -- in particular, whether they had more thought-pattern or mood-related symptoms.
The study, led by Kihwan Han, PhD, analyzed MRI scans of 54 civilians and veterans between the ages of 20 and 60 years with chronic TBI. They compared depressive symptoms using a commonly used scale of depression measurement, and they also conducted neuropsychological assessments.
Subjects with depressive symptoms showed an overall increase in connectivity between various brain regions and the amygdala, the group found. However, those who expressed a predominance of cognitive symptoms, such as thoughts of guilt, worthlessness, self-dislike, or suicidal ideation, also had reduced amygdala connectivity with prefrontal cortices of the default mode and cognitive control networks. Individuals with greater depressive affective symptoms, such as crying, loss of interest, indecisiveness, and loss of pleasure, had reduced amygdala connectivity with the brain regions of salience, attention, and visual networks.
The researchers hope the findings will illuminate changes in amygdala connectivity patterns and become a useful tool to help clinicians diagnose subtypes of depressive symptoms in traumatic brain injury and create individualized treatment plans, Han said.


.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=100&q=70&w=100)

.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=167&q=70&w=250)