Researchers from the University of Pennsylvania are reporting early success with a novel imaging technique that uses 7-tesla MRI and the amino acid glutamate as a biomarker to locate epileptic lesions in the brain that conventional MRI and other modalities may miss.
Undetected brain lesions are an issue for approximately one-third of the 65 million people worldwide who have epilepsy, are resistant to drug therapy, and are considered poor candidates for seizure-relieving surgery. To help address the problem, the researchers developed a 7-tesla MRI technique known as glutamate chemical exchange saturation transfer (GluCEST).
The technique worked well enough that if it's validated in additional trials, it could be used clinically to avoid procedures such as invasive intracranial monitoring, which is expensive and has high patient morbidity.
Glutamate's role
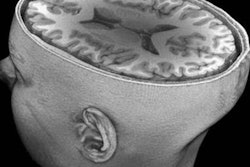
Glutamate is associated with the transmission of signals between neurons in the brain, making the amino acid a potential biomarker for identifying abnormal regions, which could trigger epileptic seizures. More specifically, seizures often originate in the temporal lobes of the brain, which include the right and left halves of the hippocampus. Depending on the person, the epileptic foci can be on the left side or right side of the hippocampus.
GluCEST relies on the chemical properties of glutamate to visualize water molecules at a very high resolution. The researchers use 7-tesla MRI to achieve the high resolution and increase the MR signal from the water molecules surrounding the chemical to indicate increased levels of glutamate.
 Ravinder Reddy, PhD, from the University of Pennsylvania.
Ravinder Reddy, PhD, from the University of Pennsylvania."Traditionally, when these patients come to the clinic, we do a battery of tests and some invasive procedures to look for which hemisphere of the brain the seizures are coming from," said Ravinder Reddy, PhD, a professor of radiology and director of the university's Center for Magnetic Resonance and Optical Imaging.
The tests could include multimodality structural and functional imaging with 3-tesla MR, FDG-PET, SPECT, and magnetoencephalography.
"With traditional MRI, we cannot see these foci, but with glutamate MRI we are seeing it because there is good accumulation of glutamate in the epileptic foci," Reddy told AuntMinnie.com. "If this [imaging technique] works out, we are avoiding a procedure by seeing which part of the brain is lighting up. Then we can decide whether to take this patient to surgery or not."
To evaluate GluCEST, Reddy and colleagues analyzed four epilepsy patients (mean age, 40 years) with drug resistance and no apparent lesions, comparing them with 11 healthy control subjects (mean age, 35 years). The authors reported their findings in Science Translational Medicine (October 14, 2015, Vol. 7:309, pp. 309-314).
All 15 subjects were imaged on a 7-tesla whole-body MRI scanner (Siemens Healthcare) with a 32-channel phased-array head coil. Two epileptologists, who were blinded to patient information, then performed independent visual analyses of the bilateral hippocampal images.
The glutamate effect
GluCEST scans revealed greater concentrations of glutamate in the ipsilateral hippocampus than in the contralateral hippocampus among all four epilepsy patients, meaning the imaging technique consistently identified the area of the brain where the epileptic seizures originated.
The results were confirmed by electroencephalography. As for the 11 healthy individuals, the GluCEST imaging technique showed normal glutamate levels in both sides of the hippocampus.
"It is a very preliminary study with the four subjects, but it's very promising," Reddy said. "With the blinding of the readers, there was very good correlation -- 100% agreement -- with the clinical findings."
While glutamate is key to the GluCEST technique, the magnet strength of 7-tesla MRI is also a must.
"One of the issues is that this technique works at 7 tesla, because we do not have enough sensitivity to detect [the epileptic foci] at 3 tesla," Reddy explained. "Technical considerations at this point limit our ability to measure activity, but I don't rule out that in the future [GluCEST with 3-tesla MRI] might be possible. But at this point, it is restricted to 7 tesla."
The subjects in the study tolerated the 7-tesla magnet very well; there were some minor cases of nausea, which can also occur with 3-tesla MRI, he added.
Future research
"If validated in a larger population of epilepsy patients, GluCEST imaging could reduce the need for invasive intracranial monitoring, which is associated with morbidity, mortality, and expense," Reddy and colleagues wrote. "In addition, GluCEST measures may yield prognostic information that can help physicians and patients determine the best form of treatment," which could include surgery or laser ablation therapy.
GluCEST's ability to detect seizure foci "could potentially improve patient care and quality of life in epilepsy patients, and sharing these results may expedite validation of this technique," the authors added.
They also cited several advantages of GluCEST over MR spectroscopy (MRS), which uses glutamate to measure brain activity. GluCEST has higher spatial resolution, which could allow better visualization of targeted brain regions, and it could also improve upon MRS' "time-intensive" image acquisition process.
Reddy and colleagues are continuing their research by developing 3D imaging to view epileptic lesions across the hippocampal regions. If and when that is accomplished, he expects it will become part of the university's routine clinical protocol.