When more than 200 people in Singapore were afflicted simultaneously with group B streptococcal (GBS) bacterium and acute central nervous system (CNS) infections, Singaporean healthcare professionals had to act quickly. Their first move was to turn to diffusion-weighted MRI (DWI-MRI) for answers.
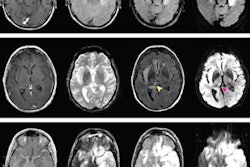
Through DWI-MRI, they discovered increased hyperintensities that illustrated lesions in certain regions of the brain that were caused by the GBS bacteria and linked to the CNS infections. Most significantly, DWI outperformed several other MR imaging techniques that did not detect any abnormalities. Eventually, the infections were traced back to the consumption of raw freshwater fish.
"Incorporating the advanced MRI technique of DWI into routine practice will enable doctors to detect abnormalities that might not otherwise be seen using other conventional methods," said co-author Dr. C.C. Tchoyoson Lim from the National Neuroscience Institute in Singapore. "Our research shows that DWI can accentuate abnormalities caused by the GBS infection and help doctors and radiologists make a more accurate diagnosis."
Going raw
GBS is a common bacterium known to cause illness in the gastrointestinal region, reproductive organs, and urinary tract. It is also known to cause bacteremia and meningitis in neonates and pregnant women. Because it rarely causes disease in healthy adults, there is a paucity of research on food-borne GBS infection.
In early 2015, Singaporean health officials were alerted to an unusual outbreak of GBS infection. Before December 2014, the number of adult GBS infections in Singapore averaged 2.9 cases per week. In the following six months, from January to June 2015, there were 238 reported cases. By July, the GBS outbreak was linked to the consumption of raw freshwater fish.
Coinciding with the rise in GBS cases, the Singapore Neurologic Infections Program (SNIP) noticed an increase in the number of CNS infections. Curious to see if there was a possible connection between the GBS outbreak and acute CNS cases, SNIP identified 14 adult patients who presented with CNS infection and also carried the food-borne GBS bacteria.
"From past experience, we found that MRI could be successfully performed in very sick patients with infection," Lim wrote in an email to AuntMinnie.com. "The bedside clinical suspicion based on neurological symptoms plus fever was to rule out meningitis and encephalitis and in some cases stroke. So MRI was the logical test."
In the study, published online July 29 in the Journal of Magnetic Resonance Imaging, all 14 subjects underwent 1.5- or 3-tesla MRI brain scans within two weeks (range, 1-10 days) of symptom onset. MRI protocols included diffusion-weighted imaging, fast spin-echo T2-weighted imaging, fluid-attenuated inversion recovery (FLAIR), and susceptibility weighted imaging.
Most of the patients presented with fever and headache, and a few had stroke-like symptoms. The group had a median age of 58 years (range, 22-81 years). Eight patients were diagnosed with meningoencephalitis, which is an infection or inflammation of the brain that mimics meningitis and/or encephalitis.
DWI discoveries
Thirteen (93%) of the subjects had abnormal findings, including increased hyperintensities in the brain parenchyma, subarachnoid space, and ventricles on DWI scans.
DWI hyperintensities in the brain parenchyma suggest the possibility of cerebral infarction, the authors noted, and were evident within 10 days of symptom onset. Abnormalities in the subarachnoid space and lateral ventricles are consistent with meningitis caused by GBS.
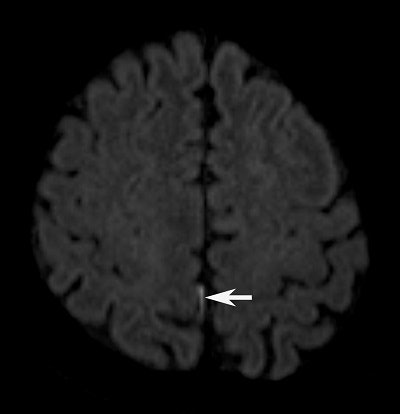 DWI pinpoints a tiny hyperintensity spot (arrow) in the posterior right fissure. Image courtesy of Dr. C.C. Tchoyoson Lim.
DWI pinpoints a tiny hyperintensity spot (arrow) in the posterior right fissure. Image courtesy of Dr. C.C. Tchoyoson Lim.DWI also found uncommon hyperintensities in the cerebellum of five patients, detecting lesions as small as 7 mm and as large as 42 mm. Interestingly, lesions in the brain parenchyma, subarachnoid space, ventricles, and cerebellum were not visible on T2-weighted or FLAIR images or with the addition of contrast.
"We were a bit surprised to discover central nervous system MRI changes in patients who ate contaminated raw fish, rather than gastrointestinal abnormalities," Lim said. "In most cases, DWI was the only abnormal finding when all else looked normal, especially to detect small amounts of pus in the ventricles and subarachnoid space."
Based on the results, the researchers recommend that DWI be added to standard MRI protocols for suspected brain infections because it helps detect subtle brain abnormalities and does not add much scan time.
"Our findings demonstrate that such patterns of DWI features can alert radiologists to disease outbreaks in the future, and that MRI adds value to multidisciplinary teams in surveillance of diseases that cross the species barrier," he said.
Lim and colleagues are also working separately on the imaging features of septic arthritis, in collaboration with clinicians and microbiologists from multiple disciplines and multiple hospitals.
"It truly takes a village!" he told AuntMinnie.com.