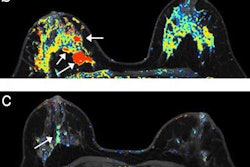
Diffusion-weighted MR images (DWI-MRI) acquired 12 weeks after the start of neoadjuvant chemotherapy for breast cancer may provide the best indication of how patients will respond to treatment, according to a study published online September 4 in Radiology.
Previous studies have shown that the apparent diffusion coefficient (ADC) -- a marker of cellular water mobility -- can significantly differentiate between breast cancer patients who will respond to treatment and those who will not, wrote the researchers led by Savannah Partridge, PhD, from the department of radiology at the University of Washington. However, results have varied in terms of using breast DWI-MRI for monitoring treatment.
In this prospective study, known as the American College of Radiology Imaging Network (ACRIN) 6698 trial, the researchers analyzed 242 participants (mean age, 48 ± 10 years). Subjects were randomized to receive 12 weekly doses of paclitaxel with or without an experimental agent, followed by 12 weeks with four cycles of anthracycline.
The MRI protocol included T2-weighted imaging, DWI, and dynamic contrast-enhanced (DCE) sequences, with 70% of the scans performed at 1.5-tesla field strength. MRI scans were performed before treatment and again during early treatment, at three weeks (227 women, 94%); during midtreatment, at 12 weeks (210 women, 87%); and after treatment and before surgery (186 women, 77%).
The researchers then calculated tumor ADC change as a percentage from pretreatment to each follow-up scan. DWI-MRI's ability to predict pathologic response was assessed with the area under the receiver operating characteristic curve (AUC) for all patients and according to their tumor hormone receptor (HR)/human epidermal growth factor receptor 2 (HER2) disease subtype.
After treatment, 80 patients (33%) achieved complete pathologic response. Overall, scans performed at two key time points -- at 12 weeks and after treatment -- were significantly predictive of treatment response. Changes in ADC after three weeks of treatment were not predictive of a complete response.
| Mean change in ADC on DWI-MRI at different treatment time points | |||
| 3 weeks | 12 weeks | After treatment | |
| Had complete response to treatment | 18% | 50% | 64% |
| Did not have complete response | 16% | 36% | 50% |
| p-value | 0.48 | 0.017* | 0.013* |
Across the four disease subtypes, the change in ADC at 12 weeks predicted treatment response only for HR+/HER2- tumors (AUC = 0.76) (p = 0.001).
"This [finding] may have special clinical importance, as HR+/HER2- tumors are less likely to shrink in response to chemotherapy and less often achieve complete pathologic response, while residual disease is also more commonly underestimated at DCE-MRI in HR+/HER2- tumors," the authors wrote.
Partridge and colleagues also tested a model that combined change in ADC with tumor subtype to improve treatment response prediction. Once again, the 12-week mark proved advantageous: At that time point, change in ADC with the two-factor model (AUC = 0.72) better predicted treatment response than change in ADC alone (AUC = 0.57) (p = 0.032).
Based on the results, the group recommended additional research "to assess the potential role of DWI-MRI as a noncontrast alternative to DCE-MRI for midtreatment assessment of therapeutic efficacy."



.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=100&q=70&w=100)


.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=167&q=70&w=250)











