Virtual 3D models of the knee based on MRI scans of anterior cruciate ligament (ACL) tears revealed which regions in the knee were most likely to develop osteoarthritis in a new study, published online in Clinical Biomechanics. The technique could help individualize rehabilitation strategies for patients following ACL surgery.
In the proof-of-concept study, researchers from various institutions throughout Finland and the U.S. collaborated on developing a method for predicting osteoarthritis in patients with knee joint injuries that would be viable for clinical use (Clin Biomech, August 9, 2019).
One of the most common knee joint injuries for athletes is an ACL tear, which is generally repaired through surgical reconstruction. In many cases, however, the initial injury is associated with damage to the cartilage that can eventually lead to joint pain, reduced mobility, and osteoarthritis.
Several techniques currently exist for predicting which parts of the knee joint appear to be most susceptible to future osteoarthritis after ligament rupture, but most of these methods either provide insufficient information or are too convoluted for clinical use, noted lead author Paul Bolcos, a doctoral student from the University of Eastern Finland, in a statement from the university.
Balcos and colleagues explored the possibility of using simplified computational modeling to assess osteoarthritis risk after knee joint injuries. To achieve this goal, they acquired MRI scans and motion capture data of two patients who had undergone ACL reconstruction surgery. Then they used these scans and data to generate virtual 3D models of the patients' knee joints.
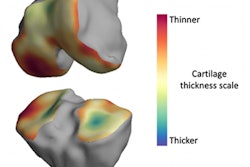
The researchers applied a series of mathematical equations to these models that allowed them to simulate knee joint movement and also recognize potential anatomical changes after the application of varying amounts of force. The simulations highlighted areas in the patients' knee joints that were most susceptible to collagen damage and cartilage degeneration.
In the first patient, for example, the modeling technique revealed that roughly 14% of the lateral tibial cartilage and 7% of the lateral femoral cartilage were likely to degenerate over the course of several years. For the second patient, the model predicted collagen damage and cartilage degeneration in the medial tibial and femoral cartilage, as well as in the posterior side of the medial joint, but not in the lateral tibial and femoral cartilage.
These predictions held up when compared with structural and compositional changes in the patients' knee joints noted on follow-up MRI scans taken three years after surgery, the group found.
"Our results suggest that a relatively simple finite element model, in terms of geometry, motion, and materials, can identify areas susceptible to osteoarthritis, in line with measured changes in the knee joint from MRI," Bolcos said. "Such methods would be particularly useful in assessing the effect of surgical interventions or in evaluating nonsurgical management options for avoiding or delaying osteoarthritis onset and/or progression."
Down the line, the modeling technique could provide a pathway to patient-specific clinical evaluation of osteoarthritis risks in those with ACL tears and indicate optimal rehab protocols, the authors concluded.