COVID-19 often initially presents as respiratory disease, but it also has serious nonpulmonary manifestations, according to a session held on July 16 at the virtual edition of ECR 2020.
In the presentation, experts from Spain, Germany, and Italy weighed in on the neurologic, cardiovascular, and pediatric involvement of COVID-19, outlining imaging's role in diagnosing and tracking these nonpulmonary manifestations.
Need-to-know neurology
Neurologic manifestations of COVID-19 are common, caused perhaps by direct infection of the virus or the body's immune system reaction, Dr. Alejandro Rovira-Cañellas of the University Hospital Vall D'Hebron in Barcelona, told session attendees.
"Which are the mechanisms that produce central nervous system damage? One proposal is the direct invasion of the olfactory tract," he said. "Another is that it invades the brain stem or that it prompts a severe immune system reaction."
Symptoms of COVID-19 may include headache, loss of smell or taste, and stroke, as well as coma, agitation, delirium, dizziness, seizure, encephalopathy, and generalized weakness. A third of patients present with headache, according to Rovira-Cañellas.
"Imaging isn't necessarily required for headache, unless additional findings are present -- red flags such as neurological deficits, fever, or patients who have not responded to initial treatment," he said. "In these cases, imaging can help exclude meningitis, encephalitis, vasculitis, or tumor."
Anosmia and ageusia are also frequent but aren't specific to COVID-19; they tend to improve after four weeks in most cases, and imaging isn't indicated, Rovira-Cañellas said.
Stroke and vascular events are common in hospitalized patients, with the most common condition being ischemic stroke, for which the rate is higher among COVID-19 patients compared with those with the flu, he said. Look for elevated inflammatory markers and infection in the endothelial cells.
"COVID-19 patients are clot formers," he said. "Most thromboembolic manifestations are cardioembolic, and large-vessel disease."
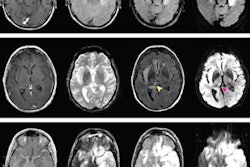
On brain MRI, COVID-19 patients may demonstrate medial temporal lobe abnormalities, nonconfluent and confluent multifocal white matter lesions, acute hemorrhagic necrotizing encephalopathy, and white-matter microhemorrhages, Rovira-Cañellas said.
Cardiovascular complications
COVID-19 patients with a predisposition for thromboembolic disease present with active inflammation, said Dr. Karl-Friedrich Kreitner, PhD, of the Johannes Gutenberg University of Medicine in Mainz, Germany.
 Dr. Karl-Friedrich Kreitner, PhD.
Dr. Karl-Friedrich Kreitner, PhD."Virally driven hyperinflammation with cytokine release may lead to vascular inflammation, hypercoagulable status, and propensity for disseminated intravascular coagulation," he said.
Patients at risk of thromboembolic disease tend to have high D-dimer levels and fibrin degradation products (FDP) -- and this is associated with death from COVID-19, Kreitner noted.
"Markedly elevated D-dimer and FDP are common in nonsurvivors of COVID-19," he said.
Cardiovascular involvement can dramatically impact prognosis of COVID-19 patients, and it's important to track D-dimer and other biomarkers while patients are in the hospital. But imaging also has its role to play, according to Kreitner.
"Initiate timely imaging in case of suspected thromboembolism," he said.
Pediatric manifestations
 Dr. Paolo Tomà.
Dr. Paolo Tomà.Finally, Dr. Paolo Tomà of Bambino Gesù Children's Hospital in Rome described how COVID-19 can appear in children. At his hospital 2,000 children were screened for SARS-CoV-2 virus with RT-PCR between March 15 and June 4; of these, 76 tested positive. And the virus can remain even after respiratory symptoms resolve, he said.
"Viral positivity can persist for as long as 47 days after symptom onset," he said.
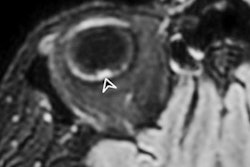
Although the disease tends to be less severe in children, these patients can develop more severe, hyperinflammatory forms of the illness such as single or multiorgan dysfunction, Kawasaki-like disease, myocarditis, and serositis. Echocardiography, ultrasound, and chest CT illuminate the disease's progression, Tomà concluded.



.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=100&q=70&w=100)



.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=167&q=70&w=250)











