MRI shows that COVID-19 can have a negative impact on the eyes of people with severe forms of the disease, according to a study published February 16 in Radiology.
The findings point to a need for follow-up screening for potentially severe ophthalmological manifestations of COVID-19 in patients who have contracted the illness, wrote a team led by Dr. Augustin Lecler, PhD, of Rothschild Foundation Hospital in Paris, France.
"Screening of [COVID-19] patients might be suitable to provide appropriate treatment and improve the management of potentially severe ophthalmological manifestations [of the disease]," the team wrote.
SARS-CoV-2, the virus that causes COVID-19, primarily attacks the lungs but has also been associated with eye conditions such as conjunctivitis and retinopathy, the authors noted. Although eye abnormalities in COVID-19 patients have been documented on MRI, research on the characteristics and frequency of these eye complications is limited.
This study, conducted under the auspices of the French Society of Neuroradiology (SFNR), included 129 patients with severe COVID-19 confirmed by reverse transcription polymerase chain reaction (RT-PCR) who underwent brain MRI scans for a variety of reasons (delayed awakening despite the discontinuation of sedation, 67%; agitation and confusion after awakening, 22%; and agitation and hallucinations, 11%). Patients were treated at 16 hospitals between March and May 2020.
The investigators found that nine (7%) of the COVID-19 patients had abnormal MRI findings on the globe, or eyeball, with one or more nodules on the posterior pole. All these patients had nodules in the macular region, or the area of the eye responsible for central vision, and eight had nodules in both eyes (89%).
Why the nodules formed in these patients is unclear, although Lecler and colleagues hypothesized it could be due to inflammation caused by the virus or to inadequate draining of veins in the eyes in patients who spend time in the intensive care unit (ICU) in a prone position or intubated. In fact, eight of the nine patients who had abnormal eye findings on MRI were admitted to the ICU, and seven of these were in the prone position in the ICU for long periods, the group noted.
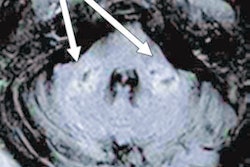
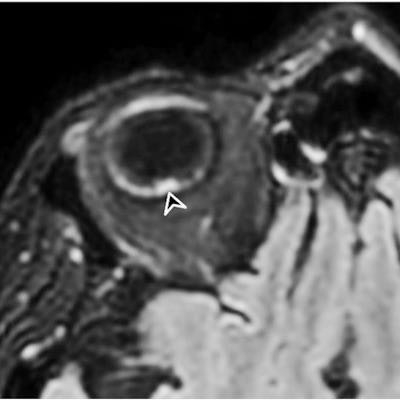
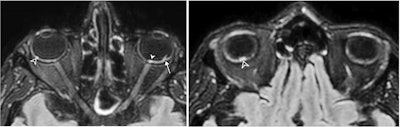 A 56-year-old man presenting with severe COVID-19. The patient had been hospitalized in the ICU for 20 days when an MRI was performed due to delayed awakening despite discontinuation of sedation. He presented with acute respiratory distress syndrome and was intubated on high-flow supplementary oxygen and placed in the prone position. 3D fluid-attenuated inversion recovery-weighted MRI reformatted in the axial plane shows several hyperintense nodules of the posterior pole of the globe located in the macular region (white arrowhead) and the extramacular region (black arrowheads). Note the presence of a focal temporal retinal detachment of the left eye (arrow). Images and caption courtesy of the RSNA.
A 56-year-old man presenting with severe COVID-19. The patient had been hospitalized in the ICU for 20 days when an MRI was performed due to delayed awakening despite discontinuation of sedation. He presented with acute respiratory distress syndrome and was intubated on high-flow supplementary oxygen and placed in the prone position. 3D fluid-attenuated inversion recovery-weighted MRI reformatted in the axial plane shows several hyperintense nodules of the posterior pole of the globe located in the macular region (white arrowhead) and the extramacular region (black arrowheads). Note the presence of a focal temporal retinal detachment of the left eye (arrow). Images and caption courtesy of the RSNA.The study results highlight the need for follow-up eye health screening in patients with severe COVID-19, which could consist of imaging the eyes with high-resolution MRI; fundoscopy to assess the back of the inside of the eye; or optical coherence tomography, which visualizes the eye's structure, according to Lecler's team.
The study should help radiologists offer COVID-19 patients even better care due to an awareness of potential ocular complications, wrote Dr. Claudia Kirsch of Zucker Hofstra School of Medicine at Northwell in Manhasset, NY, in an accompanying editorial.
"Ocular pathology from the SARS-CoV-2 virus often signifies a more severe disease process and may be occurring with greater prevalence than currently reported and visually underappreciated on current MRI," she wrote. "This article reminds all radiologists to pay attention to the orbits on MRI, especially in patients critically ill with COVID-19 admitted to intensive care."