Imaging findings on brain MRI show that COVID-19 patients may be vulnerable to leukoencephalopathy -- diseases of the brain's white matter -- according to a February 17 study in the American Journal of Roentgenology.
Although this particular neurologic manifestation of COVID-19 is uncommon, radiologists should be aware that it's a possibility, wrote a team led by Dr. Colbey Freeman of the University of Pennsylvania.
"Increasingly, effects of COVID-19 on the brain are being reported, including acute necrotizing encephalopathy, infarcts, microhemorrhage, acute disseminated encephalomyelitis, and leukoencephalopathy," the team noted.
There are currently no criteria for defining COVID-19-related disseminated leukoencephalopathy (CRDL), Freeman's group noted, so it sought to explore whether there are particular imaging findings that can help diagnose the condition.
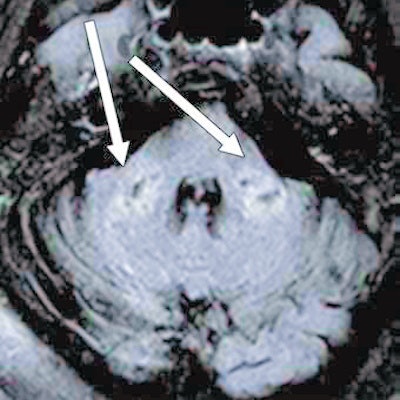
Their research included 2,820 COVID-19 patients admitted to the hospital between March and June 2020. Of these, 59 (2.1%) underwent brain MRI. Exams were considered suggestive of COVID-19-related disseminated leukoencephalopathy if they showed "white matter abnormalities atypical for other causes (such as chronic small vessel ischemic changes or infarcts) and in atypical locations (such as the bilateral middle cerebellar peduncles and corpus callosum)."
 Axial fluid-attenuated inversion-recovery MR image shows T2 prolongation in bilateral middle cerebellar peduncles (arrows). Findings were associated with restricted diffusion and areas of T1 hypointense signal without enhancement or abnormal susceptibility. Image and caption courtesy of the American Roentgen Ray Society (ARRS) and the American Journal of Roentgenology (AJR).
Axial fluid-attenuated inversion-recovery MR image shows T2 prolongation in bilateral middle cerebellar peduncles (arrows). Findings were associated with restricted diffusion and areas of T1 hypointense signal without enhancement or abnormal susceptibility. Image and caption courtesy of the American Roentgen Ray Society (ARRS) and the American Journal of Roentgenology (AJR).In the 59 patients who underwent brain MRI, the group found the following neurological conditions:
- 23 (39%) had white-matter lesions of small vessel ischemic disease.
- Six (10.2%) had acute infarcts.
- Four (6.8%) had subacute infarcts.
- Four (6.8%) had chronic infarcts.
- Three (5.1%) had white-matter lesions from multiple sclerosis.
- Two (3.4%) had microhemorrhage in association with chronic infarcts.
- Two (3.4%) had microhemorrhage associated with acute or subacute infarcts.
- One (1.7%) had abnormal basal ganglia signal from hypoxemia.
However, the team also found that six patients, or 10.2% of those who underwent brain MRI scans, had imaging findings that suggested COVID-19-related disseminated leukoencephalopathy, which manifested as "white matter lesions atypical for other causes, such as hypoxic injury, delayed posthypoxic leukoencephalopathy, chronic small vessel ischemic disease, and infarction," the authors wrote. Most of these six patients also had comorbidities, with four having hypertension and three having type 2 diabetes.
The researchers conceded that their study was limited by the fact that criteria for COVID-19-related disseminated leukoencephalopathy are lacking and that findings that might suggest the condition could overlap with findings that indicate other disease. But it's worth keeping COVID-19-related disseminated leukoencephalopathy in mind when reading these patients' MRIs, according to the investigators.
"CRDL is rare, limiting our ability to assess the full array of possible findings," they concluded. "Nevertheless, leukoencephalopathy represents an uncommon, but important, differential consideration in patients with COVID-19 with neurologic manifestations."