Preoperative MRI may lead to better planning for breast cancer surgeries, according to research presented on Sunday at the virtual RSNA 2020 meeting. One team found three MRI features tied to surgical success, while another group showed how preoperative MRI could reduce repeat surgeries.
The presentations, given by Drs. Ah Reum Park from the University of Ulsan College of Medicine in South Korea and Shinn-Huey Chou from Massachusetts General Hospital, showed the promise of MRI to help patients and their physicians pick the best breast surgery from the start. They were part of a November 29 scientific session focused on the use of MRI for breast imaging.
"MRI is well known for its high sensitivity," Park said in her presentation. "However, the role of preoperative breast MRI in newly diagnosed breast cancer remains controversial."
Preoperative MRI may reduce repeat surgeries
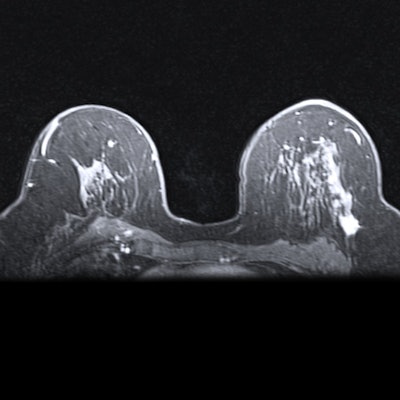
Park and her research team evaluated the benefits of presurgical MRI for young women with breast cancer. Their retrospective study analyzed data from 964 women diagnosed with breast cancer at age 35 or younger.
Out of the patients, roughly two-thirds opted for preoperative MRI, while the remaining one-third proceeded to surgery after mammography. The researchers used inverse probability-weighted analysis to account for differences between the two groups and propensity score to adjust for potential confounding variables.
In the adjusted analysis, women who opted for presurgical MRI had higher odds of undergoing mastectomy as their first surgery, but they were less likely to need repeat surgery. Despite a higher number of initial mastectomies, the MRI group also had a similar number of total mastectomies to women who did not undergo presurgical MRI.
"We found that preoperative breast MRI was associated with a reduction in the rate of repeat surgery without an increase in the overall mastectomy rate," Park said.
MRI findings also changed the surgical plan in 15% of cases. But after reviewing the data, Park and her team deemed the changes appropriate in only 62% of cases. She cautioned that biopsies are still needed for presurgical MRI findings.
"Considering these rates of pathological justification, preoperative biopsy should be obtained for MRI-detected additional lesions to avoid overtreatment," she said.
3 MRI features tied to DCIS surgical success
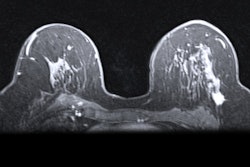
In another presentation, Chou described how her team analyzed results from a prospective, multicenter trial evaluating the use of MRI for ductal carcinoma in situ (DCIS). The team identified three MRI features that could help predict outcomes for surgical treatment of DCIS.
"Current approaches lead to the potential for both overtreatment and undertreatment," Chou said. "It is therefore critical to identify methods that accurately determine disease extent and tumor biology."
The team found lesion size on preoperative MRI was tied to the success of single wide local excision in their study of 399 women with DCIS. Successful surgeries had a median lesion size of 17 mm on MRI, compared with an average size of 24.5 mm for unsuccessful surgeries.
In addition, cancers with a low or intermediate nuclear grade on biopsy were associated with surgical success, compared with cancers with a high nuclear grade. Lesions with focal distribution of nonmass enhancement (NME) also had better success rates than those with segmental or other NME distributions.
"These results suggest that MRI features may be used to predict surgical success rates," Chou said.
MRI's ability to catch additional cancers also stood out in the study results. Almost one-third of the 66 patients recommended for biopsy based on MRI findings had additional malignancy, including six cases of invasive cancer. In addition, 39% of patients who converted to mastectomy did so because of their MRI findings.
"MRI has shown promise in improving DCIS depiction," Chou said.