MRI effectively tracks soft-tissue complications in patients who have undergone hip resurfacing arthroplasty or total hip replacement, according to research published July 7 in Clinical Orthopaedics and Related Research.
Given its performance in the study, MRI could be utilized in standard follow-up procedures for these patients, the researchers from the Hospital for Special Surgery (HSS) in New York concluded.
"The results suggest MRI is uniquely capable of assessing soft-tissue complications and that the use of MRI should be included as part of routine follow-up protocol for hip replacement patients, as an annual clinical assessment dependent on survey or blood metal ion testing alone may not detect complications," the hospital said in a statement.
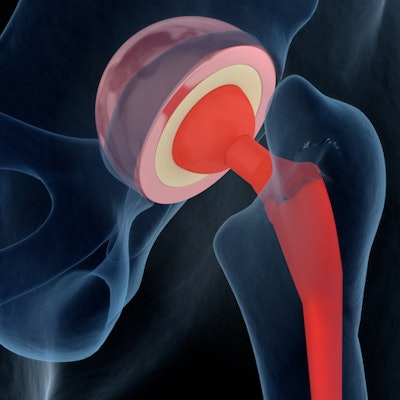
Hip replacement parts are made of plastic, ceramic, metal, or a combination of these, and through regular use may eventually wear down, according to a team led by Matthew Koff, PhD. Since particles from the replacement parts may cause damage to joint tissue, it's important to follow hip replacement patients over time. MRI is a good way to do this, especially since it doesn't impart radiation, according to the researchers.
Koff and colleagues conducted a study that used MRI to assess local tissue complications in 206 patients (both symptomatic and asymptomatic) who had undergone hip resurfacing arthroplasty or hip replacements with parts made of different materials. The group evaluated the volume of joint tissue reaction to the implants with MRI and measured levels of metal particles in the blood through blood metal ion testing.
MRI detected adverse local tissue reactions in 25% of patients who had hip resurfacing arthroplasty -- a surprising result, the investigators stated, as these patients described symptoms that were either similar to or less severe than those described by patients with total hip replacements. Koff's team also found that patients who had hip resurfacing arthroplasty had a larger volume of joint tissue reaction on MRI exam and an almost five times higher risk of tissue complications compared with patients who had ceramic-on-polyethylene hip replacements.
"We found that patients can be completely asymptomatic and have high-functioning hip scores while harboring reactions that could start to destroy the soft tissues around the hip," said study senior author Dr. Hollis Potter in the hospital statement. "This finding is important because tissue reactions typically worsen over time. Delayed detection results in unnecessary pain, longer and more complicated revision operations and more challenging recoveries."
The researchers hope that the study results will prompt clinicians to use MRI for evaluating patients after hip resurfacing arthroplasty or replacement surgery.
"By sharing our findings, we hope physicians will start incorporating MRIs into patient assessments, leading to earlier detection of issues and better outcomes," Potter said. "Widespread use of MRI to assess soft tissue damage may also help identify patterns that could ultimately improve implant design in the future."





















