Diffusion-weighted MRI (DWI-MRI) can help predict breast cancer patients' response to neoadjuvant chemotherapy, a study published January 12 in Nature Scientific Reports has reported.
Researchers led by Dr. Nathalie Hottat from Burgmann University Hospital in Brussels, Belgium, found a significant increase in breast cancer region of interest (ROI)-apparent diffusion coefficient (ADC) on diffusion-weighted imaging, as well as a decrease in the nuclear antigen Ki-67, a tumor biomarker.
"This finding could validate the reliability of the [apparent diffusion coefficient] value as a routine biomarker in assessing breast cancer response to neoadjuvant chemotherapy," Hottat and co-authors wrote.
Assessing cell proportions stained for Ki-67 helps measure breast cancer proliferation, the group noted. A high level of Ki-67 proliferation reflects high tumor aggressiveness and thus a potential sensitivity to neoadjuvant chemotherapy. This makes the Ki-67 index a biomarker for how effective treatment can be in patients undergoing the treatment.
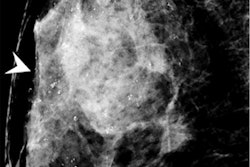
MRI has been heralded as an effective imaging method for assessing chemotherapy response and predicting pathologic response. Diffusion-weighted imaging (DWI) is a newer method that measures water movement in tissue by using diffusion-sensitizing gradients during image acquisition. Breast malignancies show restricted diffusion compared with normal breast tissue, presenting as bright spots, according to Hottat's group.
The investigators sought to compare 2D ROI-ADC measurements with the Ki-67 proliferation index before and after the women had chemotherapy. Using DWI-MRI, they analyzed any changes in the apparent diffusion coefficient as a predictive biomarker for changes in the Ki-67 index due as the result of chemotherapy.
Hottat's group conducted a study that included data from 47 women with 49 invasive breast cancers. All the women received the same neoadjuvant chemotherapy followed by surgery. MRI with dynamic contrast enhancement and DWI were performed and analyzed before and after each woman completed treatment. Out of the total, 19% of the study cohort had a complete pathologic response.
The researchers created a model for predicting variations in the Ki-67 index, tracking variables such as patient age, hormonal receptor status, human epidermal growth factor receptor 2 status, and ROI-ADC variations. They found a significant inverse correlation between the Ki-67 index and ROI-ADC before (r = -0.443) and after chemotherapy (r = -0.614).
The team also found that after chemotherapy, a significant increase in breast cancer ROI-ADC on DWI-MRI was observed, and a significant decrease in the Ki-67 index predicted.
| Correlation between Ki-67 index and ROI-ADC before and after neoadjuvant chemotherapy | |||
| Measure | Before | After | p-value |
| Ki-67 index | 45.8% | 18.0% | < 0.001 |
| ROI-ADC (with 1 as reference) | 0.883 | 1.533 | < 0.001 |
The authors suggested that changes in ADC values could serve as a surrogate marker for changes in the Ki-67 index in breast cancer treatment response.
"We recommend the systematic use of an ROI targeted at the lowest breast cancer ADC in patients before and after neoadjuvant chemotherapy," they concluded.