"Handcrafted" radiomics and deep-learning radiomics based on pretreatment MRI data help predict locally advanced cervical cancer (LACC) concurrent chemoradiotherapy treatment outcomes, according to research published January 12 in Scientific Reports.
The study results show promise for tailoring care for patients with this particular cancer, wrote a team led by Sungmoon Jeong, PhD, of Kyungpook National University, Daegu, South Korea.
"Our findings may contribute to the development of personalized treatment strategies for locally advanced cervical cancer patients," the group noted.
Cervical cancer is the fourth most common cancer and the fourth leading cause of cancer-related deaths in women around the world, the investigators wrote. Concurrent chemoradiotherapy (CRT) is the standard treatment for locally advanced cervical cancer, and consists of external beam radiotherapy and intracavitary brachytherapy with concurrent chemotherapy. But a "reliable tool for predicting CRT responses" is needed, they explained.
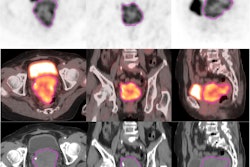
Jeong and colleagues conducted a study that included 252 locally advanced cervical cancer patients who underwent chemoradiotherapy between 2006 and 2019, dividing the group into training (167 patients) and test (85 patients) sets for a radiomics algorithm based on data from T1- and T2-weighted MR scans. The "handcrafted" radiomics model included 1,890 imaging features, while the deep-learning radiomics model consisted of a 3D convolutional neural network.
Jeong and colleagues reported that both the handcrafted and deep-learning models effectively predicted chemoradiotherapy response in patients with locally advanced cervical cancer – although the deep-learning model performed better than the handcrafted model. They also reported that adding clinical factors (i.e., age, tumor size, International Federation of Gynecology and Obstetrics [FIGO] stage, human papillomavirus infection status, pathology, and lymph node metastasis status) into the models improved the handcrafted model's area under the receiver operating curve (AUC), sensitivity, and positive and negative predictive value. Overall, the team found that 77.4% of patients had complete remission of disease at three months post-treatment.
| Performance of two models for predicting locally advanced cervical cancer treatment response | ||||
|---|---|---|---|---|
| Measure | HCR with MRI data | HCR with MRI and clinical data | Deep learning with MRI data | Deep learning with MRI and clinical data |
| AUC | 0.59 | 0.67 | 0.72 | 0.78 |
| Accuracy | 59% | 47% | 73% | 77% |
| Sensitivity | 31% | 47% | 73% | 94% |
| Specificity | 87% | 87% | 72% | 60% |
| Positive predictive value | 42% | 52% | 43% | 40% |
| Negative predictive value | 81% | 85% | 90% | 97% |
"In clinical decision-making, physicians do not rely on a single piece of information," the group noted. "To arrive at a conclusive decision, information from different categories, including medical imaging, laboratory tests, physical examinations, histopathologic, and genomic results is combined. Therefore, integrating these heterogeneously originated data might be pivotal, even in the case of radiomics prediction."
The ability to predict a patient's CRT treatment response is important and the study suggests that radiomics offer a promising way to do this, the team noted.
"Patients predicted to have a poor response can benefit from dose escalation or alternative treatments," Jeong and colleagues concluded. "Conversely, those expected to have a good response might be candidates for de-intensified treatment, thereby reducing the risk of treatment-related side effects. In other words, personalized medicine can be provided to patients with locally advanced cervical cancer."
The complete study can be found here.